At the Saethre-Chotzen syndrome is a disease associated with craniosynostosis. Saethre-Chotzen syndrome is congenital as the causes are genetic in nature. The disease is known by the abbreviation SCS. The main symptoms of Saethre-Chotzen syndrome are synostosis of the coronary suture on one or both sides, ptosis, an asymmetrical face, unusually small ears, and strabismus.
What is Saethre-Chotzen Syndrome?

© Matthieu - stock.adobe.com
The Saethre-Chotzen syndrome occurs relatively rarely. With an estimated frequency of 1: 25,000 to 1: 50,000, Saethre-Chotzen syndrome occurs somewhat more frequently than many other hereditary diseases. Craniofacial malformations are typical of Saethre-Chotzen syndrome. A craniosynostosis occurs together with a symphalangism and syndactylia.
The Saethre-Chotzen syndrome is referred to by some doctors with the synonymous terms Chotzen syndrome or Acrocephalosyndactyly Syndrome Type III designated. Basically, the common name of Saethre-Chotzen syndrome goes back to those people who scientifically described the disease for the first time in 1931. These are the two physicians Chotzen and Saethre.
In addition, there is a special form of Saethre-Chotzen syndrome, in which patients not only have typical symptoms but also abnormalities on the eyelids. This peculiarity is referred to with the term Robinow-Sorauf syndrome. As part of this disease, the patient's big toes are split or sometimes double. So far it has been assumed that the Robinow-Sorauf syndrome is an allelic variation of the Saethre-Chotzen syndrome.
causes
The factors responsible for the pathogenesis of Saethre-Chotzen syndrome are genetic defects. With regard to the development of Saethre-Chotzen syndrome, both deletions and point mutations are particularly relevant here. These faulty processes take place on the so-called TWIST1 gene. A special transcription factor is coded at the corresponding locus. This defines lines of cells and is involved in differentiation.
Due to the genetic defects in this gene, the sutures of the skull fuse too early. The deletions result in an appearance of the affected patients that deviates significantly from the average. In addition, in some cases they are responsible for the fact that some people with Saethre-Chotzen syndrome suffer from impaired mental abilities.
Symptoms, ailments & signs
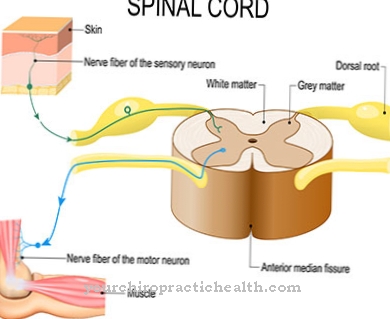
The clinical symptoms of Saethre-Chotzen syndrome vary from case to case. Typically, as newborns, the affected people have a synostosis that arises in the area of the coronary suture. This seam is also called a lambda seam or arrow seam.
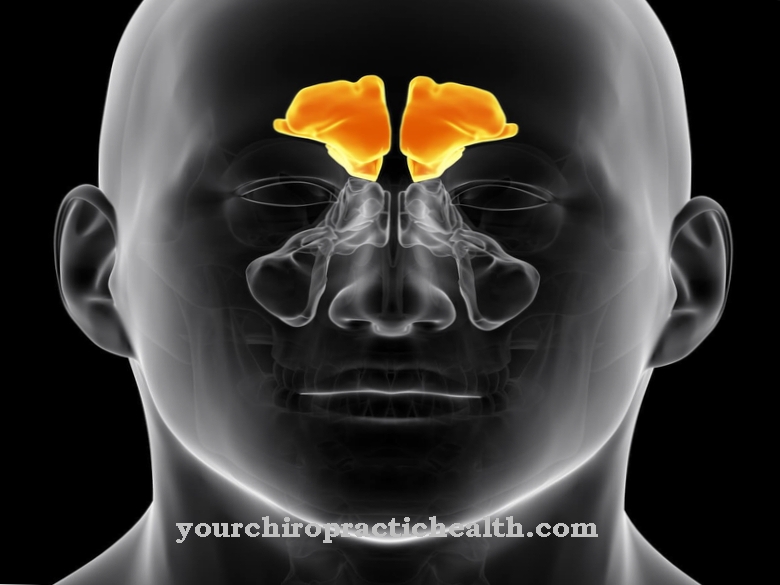
Because of this, the patient's skull has an unusual shape. In addition, there are often clear asymmetries in the face of the person. In addition, the patients usually have a very high forehead with a deep hairline, small ears and a strabismus. Ptosis, brachydactyly and stenosis of the lacrimal ducts are also common.
The middle and index fingers are often partially connected to one another in the skin area. In the majority of cases, people with Saethre-Chotzen syndrome have an average intelligence quotient. However, some of those affected show significant delays in intellectual development.
Some of the people with Saethre-Chotzen syndrome develop hearing loss during childhood. This is often a conductive hearing loss. In rare cases, in addition to the general symptoms, patients suffer from short stature, a hypoplastic upper jawbone, deformities of the heart or hypertelorism.
In addition, some of the patients show a cleft palate, malformations of the vertebral bones, uvula bifida and obstructive sleep apnea. If the synostosis is particularly pronounced, the affected patient may experience impaired vision, pain in the head area due to increased internal pressure in the skull and epileptic seizures. In extreme cases, people die as a result of their symptoms.
Diagnosis & course of disease
The diagnosis of Saethre-Chotzen syndrome is usually made by a specialist doctor. The general practitioner or the pediatrician refer the patient to the appropriate specialist. A first anamnesis in the presence of the custodial of the mostly child patients provides information about the present symptoms.
The clinical examination is based on the typical symptoms, which in some cases already strongly indicate Saethre-Chotzen syndrome. The focus is on visual examinations of the phenotype and various imaging methods. The attending physician uses, for example, X-ray and CT techniques. These usually focus on the area of the skull, extremities and the spine.
A definite diagnosis of Saethre-Chotzen syndrome is ultimately possible with the help of a genetic laboratory test. If a deletion or a point mutation is identified in the responsible gene, the diagnosis of Saethre-Chotzen syndrome is considered confirmed. The differential diagnosis also plays an important role, as some symptoms of Saethre-Chotzen syndrome are sometimes confused. The doctor rules out Crouzon syndrome, Baller-Gerold syndrome, Pfeiffer syndrome, and Muenke syndrome.
Complications
A number of complications can occur as a result of Saethre-Chotzen syndrome. Those affected typically suffer from significant delays in intellectual development. This can lead to social exclusion and, as a result, to the development of psychological complications such as depression or inferiority complexes. As a result of hearing loss, there may be further restrictions in everyday life and the quality of life of those affected is reduced.
If there are deformities of the heart, heart failure can occur as a long-term consequence. Furthermore, in the course of the disease, epileptic seizures occur repeatedly, which increase the risk of accidents. In the worst case, those affected die from the consequences of the various complaints. Even with a positive outcome, physical and mental complications inevitably arise. Surgical treatment of individual malformations is always associated with risks.
Bleeding and infections as well as nerve injuries can occur during an operation. This can lead to wound healing disorders, inflammation and scarring. The drugs prescribed to accompany the surgical treatment must be precisely tailored to the patient's condition. Otherwise, life-threatening side effects and interactions can occur due to the various mental and physical disorders.
When should you go to the doctor?
Saethre-Chotzen syndrome must always be examined and treated by a doctor. If left untreated, it can lead to serious complications that severely limit the life of the person affected. Since this syndrome is a genetic disorder, it cannot be completely cured either. The patient is therefore dependent on purely symptomatic treatment. If the person concerned wishes to have children, genetic counseling can also be carried out to prevent the syndrome from being passed on to the children.
A doctor should be consulted if the patient suffers from a significantly delayed development. Above all, intellectual development is severely restricted. A hearing loss or short stature can also indicate Saethre-Chotzen syndrome and should always be examined by a doctor. In most cases, deformities of the heart also occur, so that the person concerned is dependent on regular heart examinations.
An initial examination and diagnosis of Saethre-Chotzen syndrome can be carried out by a general practitioner or a pediatrician. However, further treatment is carried out by various specialists and depends on the severity of the malformations.
Treatment & Therapy
The patients with Saethre-Chotzen syndrome already undergo various surgical interventions in childhood. A cranioplasty is usually used. The narrowed airways are widened and the cleft palate is closed. Regular check-ups monitor hearing and intellectual and motor development. It is also important to recognize possible amblyopia in good time. The same applies to papillary edema with a chronic course.
prevention
According to the current state of research, Saethre-Chotzen syndrome cannot be prevented.
Aftercare
The scope of follow-up measures for Saethre-Chotzen syndrome (SCS) is based on the nature of the symptoms of the disease and their respective severity. Symptomatically, the SCS can cause deformations of the head, midface, spine, extremities and joints. In the majority of cases of illness, the aforementioned body parts do not develop properly. Serious secondary diseases can follow the deformation.
The task of follow-up care is to identify and treat secondary SCS diseases as early as possible. The focus of the follow-up measures is the observation of the course of the disease. Deformations in the head area, for example, are usually reshaped surgically. Blindness of the person concerned can thus be avoided. During the follow-up care of the reshaping, an ophthalmologist examines the affected person's optic nerves every quarter up to the age of 12.
The follow-up examinations aim to identify as early as possible whether and to what extent the skull is again too narrow and, if applicable, there is a risk of blindness. With the reshaping of the skull, epileptic seizures can occur in individual cases. These can be treated with medication during aftercare.
As the disease progresses, the development of epilepsy can be closely monitored neurologically using electroencephalographic recordings (EEG). Deformations in the remaining four parts of the body regularly lead to symptomatic restricted mobility. The aftercare basically focuses on increasing mobility by means of physiotherapy. Sore parts of the body are treated with medication.
You can do that yourself
The possibilities for self-help in Saethre-Chotzen syndrome are geared towards optimal handling of the disease. The patient and their relatives are exposed to various coping challenges, for which they should be prepared as extensively as possible.
The patient's self-confidence must be built up at an early stage. Due to the visual abnormalities, the disturbance represents a particular difficulty in everyday life, which the patient should be able to face emotionally. The help and support of a psychotherapist can also be used for this. Since mental abilities are restricted, consideration must be given to the child's development. A comparison with playmates of the same age is not permitted. The learning process should also be tailored to the patient's capabilities and skills.
In the course of the disease, there are often several surgical interventions in the first few years of life. To cope with these challenges, the organism should be supported with a healthy diet rich in vitamins. Optimal sleep hygiene and the avoidance of stress also help relieve symptoms. In addition to the malformations, many patients also suffer from hearing loss. This fact must be taken into account in everyday life when reducing the risk of accidents and language. Targeted training helps to improve language skills and communication with other people.

.jpg)



















.jpg)