In professional circles, the Pubic bone inflammation also as Osteitis pubis designated. The term “inflammation” is misleading insofar as the symptoms are not caused by infections. Rather, they are usually caused by repeated trauma to the affected areas through incorrect or excessive stress.
What is pubic inflammation?

© Henrie - stock.adobe.com
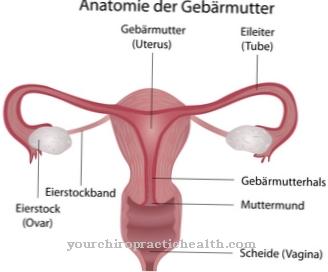
From one Pubic bone inflammation The pubic bone, the pubic symphysis (symphysis) and the structures around it are primarily affected. The pubic bone inflammation is also called Symphysenosteitis or Pubalgia designated. The pubic bone forms part of the hip bone. The other two parts are the ischium and ilium. Everyone has two hip bones and one sacrum, which in turn form the pelvis.
The so-called pubic symphysis is a combination of fibers and cartilage that connects the two pubic bones. So they are posable to a certain extent. Relaxin is released in pregnant women. This hormone ensures additional mobility of the pubic symphysis to facilitate childbirth and prevent fractures as much as possible.
Athletes are particularly hard hit by pubic bone inflammation. Up to seven percent of athletes develop the inflammation every year. The quota is highest among soccer players, tennis players and basketball players. The average age for men is 30 years. On average, women are only affected at the age of 35. Depending on the severity of the disease, the person concerned may have to forego sport for a long time and can only slowly return to training.
causes
The main cause of pubic bone inflammation is the overload and excessive stress on the symphysis. This can lead to the formation of scar tissue, which can lead to the breakdown of bones. This breakdown triggers cysts in adjacent areas. In addition, so-called stress fractures can occur. Stress-related breaks are referred to as such.
Sports with many changes of direction, sprints or shooting elements are particularly often affected, as strong tensile forces act on the pubic symphysis. In addition to the sports mentioned above, running sports and American football are also included. Athletes are therefore a special risk group.
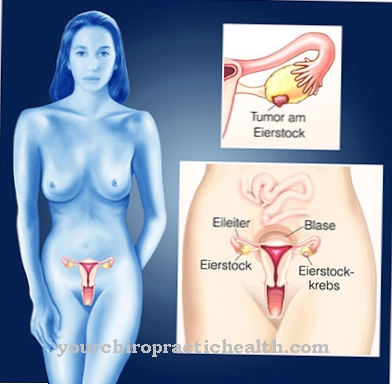
But pregnant women are also affected. Pregnancy and childbirth can also cause pubic bone inflammation. Studies have shown that after birth, bleeding in the symphysis region can occur. In some cases, the adjacent bone is also affected. Cracks in the cartilage are not uncommon.
An operation in the pelvic area can also be the cause of pubic bone inflammation. Here the inflammation occurs as a complication. Examples of this are prostate surgery or the insertion of a catheter for the bladder. This type of urinary catheter runs past the pubic bone and can also lead to an osteitis pubis.
Symptoms, ailments & signs
Various symptoms can indicate pubic bone inflammation. The swellings in the area of the symphysis are noticeable. Often times it is sensitive and responds to pressure that is associated with pain. Pain in the pubic branches and symphysis pubis is the main symptom of the disease.
Sometimes this pain is very stressful. Sports activities can no longer be carried out, depending on the case, as the inflammation leads to massive restrictions. In addition, pain can spread to the hip or groin. It is not uncommon for pubic bone inflammation to be associated with pain in the lower abdomen or the pelvic floor.
Also typical are pain when standing up after sitting for a long time. This "start-up pain" usually subsides again with uniform movements. On the other hand, climbing stairs or jerky movements often causes pain for those affected.
Diagnosis & course of disease
The diagnosis is not easy. Many sports injuries are associated with similar symptoms. The disease is often confused with groin problems such as strains. Overloading some tendons can also cause similar pain.
Pubic bone inflammation must be differentiated from avulsion fractures, bone marrow inflammation, rheumatic diseases and hernias. Sprained adductors or diseases of the urinary and genital tract can also lead to similar symptoms.
To make a diagnosis, the doctor will first ask about the symptoms and medical history. Only then will he conduct various physical examinations. Imaging can be used to diagnose pubic bone inflammation. Similar to a blood test, a distinction must be made here between inflammatory diseases.
Depending on the infection, the diseases are not always easy to distinguish. In the case of pubic bone inflammation, however, the inflammation parameters in the blood are not increased. X-rays and MRIs can also be used to differentiate.
Complications
A pubic bone inflammation usually heals without complications. However, as the disease progresses, the pain can spread and radiate to the hips, groin, lower abdomen and pelvic floor. In the case of protracted illnesses, the pain can lead to misalignments and occasionally to psychological complications. Typical of chronic diseases are, for example, depressive moods, which can develop into severe depression if the course is severe.
Surgical treatment can be associated with bleeding and impaired wound healing. Very rarely, nerve injuries occur that require further intervention. Prescribed drugs can cause side effects and interactions such as headaches, gastrointestinal complaints, edema, reddened skin and temporary visual and hearing impairments. Allergic reactions and intolerance cannot be ruled out.
With cortisone treatment, complications such as cardiovascular complaints, an increased susceptibility to infections and weight gain are possible. It can also lead to water retention in the tissue. Cortisone also promotes the development of osteoporosis. During electrotherapy, skin damage, circulatory disorders, cardiac arrhythmias, sensory disorders and other complications can occur. If you start exercising too soon after treatment, the pubic bone inflammation is likely to recur.
When should you go to the doctor?
If acute pain persists while jogging or doing sit-up exercises, the cause may be pubic bone inflammation. A doctor's visit is indicated if symptoms recur and make exercise difficult. The symptoms usually develop insidiously and should be clarified early on. It usually affects people who are active in sports and who often cycle, jog or ride a horse. Anyone who lifts heavy for work is just as at risk as pregnant women, rheumatism patients and people with pelvic obliquity. If you belong to these risk groups, it is best to see a doctor if the symptoms mentioned appear.
Affected persons consult their family doctor or an orthopedic surgeon. Other contact points are sports medicine specialists and pain therapists. In principle, pubic bone inflammation can be treated well if it is recognized at an early stage. Often, however, pubic ostitis is based on another condition that must be determined in the course of intensive examinations. In addition to the symptomatic treatment, further visits to specialists should therefore take place. The doctor must be informed about an increase in symptoms and any side effects of the prescribed pain medication.
Therapy & Treatment
As a rule, pubic bone inflammation heals on its own. If this is not the case, injection therapy or surgery can be considered. In principle, however, the inflammation is mainly treated conservatively. Sometimes it can take several months for the disease to finally heal. Pain-inducing movements and sports should at best not be carried out during the healing phase.
Patience is imperative during therapy, otherwise relapses may occur. Physiotherapy is one treatment option. Anti-inflammatory drugs like ibuprofen can also help relieve pain and provide short-term relief. Treatment with cortisone is also possible. Other options are electrotherapy and ultrasound treatments. After the inflammation has healed, it is important to start training again slowly. Avoid excessive stress on the pelvic girdle.
prevention
As a preventive measure, it is important to warm up before training in order to prevent overload as much as possible. Stretching the adductors and targeted training of the trunk and abdominal muscles reduce the risk. Any malformations in the arch of the foot can be adjusted with insoles. This prevents incorrect appearance and minimizes the risk of pubic bone inflammation due to improper stress.
Aftercare
If the pubic bone inflammation has been cured well, a one-time follow-up examination is sufficient. The doctor must clarify whether the patient still has symptoms. Prescribed drugs must be gradually discontinued after recovery. Depending on whether anti-inflammatory drugs or stronger medication have been prescribed, the tapering off must be monitored by a doctor. After cryotherapy or electrotherapy, psychological support may be useful for the patient.
The doctor will usually recommend a break from exercise. After a pubic bone inflammation, intensive physical exercise should be avoided for at least one to two weeks. After an operation, follow-up care takes place in the hospital. If curettage has been used, the surgical wound must be carefully observed.
Competitive athletes need intensive aftercare after pubic bone inflammation. Otherwise, the complaints can reappear and significantly reduce performance. On the one hand, recurring illnesses can be avoided through early therapy. On the other hand, extensive follow-up care is necessary.
The orthopedic surgeon or general practitioner will take care of the aftercare for a pubic bone inflammation. In the case of intense pain that radiates into the lower abdomen and pelvic floor, further treatment by a pain therapist is usually necessary. If necessary, the physiotherapist is also involved in the follow-up care.
You can do that yourself
The pubic symphysis is a neuralgic point of the human body, which especially competitive athletes have to notice regularly. Inflammation of the pubic bone or the pubic symphysis results almost exclusively from continued overload. The best self-help measure is therefore not to constantly overwhelm the body, but to adapt the training to your own condition and your own physical performance. In particular, short, fast movements, hooking or sprinting with abrupt stops put excessive strain on the pubic bone. If such behavior cannot be avoided, which should only be the case with professional athletes, countermeasures must be taken regularly.
Physiotherapeutic measures can help to strengthen and relieve the stressed body region. Very often, however, it is necessary for those affected to take a longer rest phase in which they do no or only light endurance sports. Anyone who lifts heavily at work may have to take a long break or pursue another activity. Those affected should follow the instructions of their attending physician, otherwise pubic bone inflammation can be very persistent or even chronic. The pain associated with inflammation can usually be treated well with over-the-counter anti-inflammatory drugs such as ibuprofen.

.jpg)
.jpg)


















.jpg)



