As Vaginal cancer or Vaginal cancer is a malignant tumor of the female vagina, which occurs very rarely. A distinction is made between several types, with the so-called squamous cell carcinoma being the most common tumor with over 90 percent of cases. In the remaining ten percent of cases, either black skin cancer or adenocarcinoma are the triggers for the vaginal cancer.
What is vaginal cancer?
.jpg)
© Alila Medical Media - stock.adobe.com
The medical professionals call that Vaginal cancer also as Vaginal cancer - This disease mainly affects women between the ages of 60 and 65.
A distinction is made between primary and secondary vaginal cancer, with the latter occurring much more frequently. In this case, the tumors develop from other neighboring organs - very often vaginal cancer is preceded by cervical cancer.
In primary vaginal cancer, on the other hand, it develops directly from the cells of the vagina. Vaginal cancer is a very rare disease - only about one to two percent of all malignant tumors of the female genital organs are vaginal cancer.
causes
The causes of vaginal cancer are diverse and in some cases still unexplored - one of the main known causes, however, is infection with the so-called human papilloma viruses. These are the triggers for numerous sexually transmitted diseases.
Diethylstilbestrol, also called DES for short, is considered to be another cause of vaginal cancer. This was given to women during pregnancy until it was banned in 1971 to prevent miscarriage.
Women who have taken this artificial estrogen are significantly more likely to develop vaginal cancer because the effect of this drug is protracted. This means that vaginal cancer can break out years or even decades after taking the hormone.
Symptoms, ailments & signs
Vaginal cancer proceeds without any clear signs of illness at the beginning. In the first stages, unspecific symptoms such as increased vaginal discharge, heavy intermenstrual bleeding or an unusual feeling of pressure in the vagina occur. These abnormalities can indicate vaginal cancer, but they often have harmless causes.
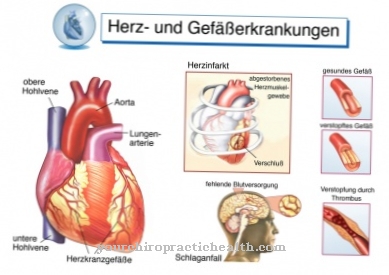
As the disease progresses, the result is increasing bleeding and pain. These occur mainly during sexual intercourse and when urinating and quickly subside. Larger carcinomas make urination and bowel movements difficult. Affected women also suffer from severe nerve pain that can be localized on the back or legs.
At the same time, sensory disturbances or symptoms of paralysis in the limbs often occur. Untreated cancer progresses and eventually spreads to neighboring tissues and surrounding organs. The cervix, urinary bladder, outer vagina and rectum are particularly affected, but also lymph nodes, liver, lungs and bones.
Very large carcinomas can cause circulatory disorders, urinary obstruction and other complications. With timely therapy, secondary symptoms of this kind can be avoided. After the carcinoma has been removed, the symptoms usually subside quickly. Vaginal cancer is usually not visible externally.
Diagnosis & course
Vaginal cancer is usually not clearly recognizable due to individual symptoms. In some women, vaginal cancer can cause bleeding after intercourse or a discharge, but these symptoms are also possible in numerous other diseases.
It is only in the advanced stages of the disease that vaginal cancer causes bulging pain or disorders of the urinary bladder or intestine. Vaginal cancer is therefore usually detected by chance during preventive examinations at the gynecologist. The gynecologist takes a tissue sample, the so-called cell smear, from the mucous membrane of the female vagina.
This is examined in the laboratory - during this examination, vaginal cancer can usually be clearly diagnosed. If vaginal cancer has been found, it must now be determined how far it has already spread and whether it has metastasized in other organs. The cervix, rectum, and bladder are often affected; the metastases radiate into the lungs, liver or bones rather less often.
Complications
In the worst case, the disc cancer spreads to other parts of the body. Then tumors can grow into the neighboring organs - i.e. cervix, vulva, urinary bladder and rectum - or spread via the lymphatic system. The metastases rarely settle in the liver, lungs and bones. Expansion into the pelvis can cut off other organs from the blood supply.
If the ureters are affected, the urine can flow out poorly or not at all. Urine congestion and severe kidney damage are the result. In general, malignant tumors also cause physical degradation, which reduces quality of life and affects mental health. Surgical removal of the tumors can injure neighboring organs or anatomical structures. This can lead to bleeding and secondary bleeding.
Injuries to the nerves result, among other things, in functional impairment of the urinary bladder. Due to the colonization of germs in the vagina, inflammation occurs relatively often, which in turn can lead to inflammatory connecting ducts (fistulas) between the urethra and the urinary bladder. Loss of function and allergic reactions cannot be ruled out. Vaginal cancer also tends to recur months or years after treatment is finished.
When should you go to the doctor?
Vaginal cancer must always be treated by a doctor. In the worst case, the cancer can spread to other areas of the body and lead to various complaints or complications. If the vaginal cancer is not treated, the life expectancy of the person affected may also be limited by the disease. A doctor should always be consulted if the person concerned suffers from heavy intermenstrual bleeding. These occur relatively frequently and are usually very strong.
In some cases, there may also be pain during intercourse, although the pain may also occur when urinating. Vaginal carcinoma is not infrequently also noticeable through sensory disturbances, so that a doctor should be consulted. Often there are also disturbances of the blood circulation or even an obstruction of urine. If these symptoms occur, a urologist or gynecologist must be consulted. Further treatment usually takes place surgically in a hospital. An early diagnosis has a positive effect on the further course of the disease.
Treatment & Therapy
The success of the treatment at Vaginal cancer depends primarily on when the disease is recognized and when treatment is started. Of course, the sooner treatment begins, the better the chances of a complete cure.
As a rule, an attempt will be made to surgically remove the tumor. If this is still in the early stages, this is usually possible without major problems and the vagina can be preserved. Sometimes, however, a complete removal of the vagina or other organs such as parts of the bladder or intestine is necessary.
A possible treatment method for vaginal cancer is radiation or a combination of both treatment methods. When it comes to radiation, doctors differentiate between two treatment methods - radiation from the inside and radiation from the outside. In contrast to other types of cancer, chemotherapy is rarely used.
prevention
The disease can be prevented directly Vaginal cancer barely. However, it is especially important for women over the age of 50 to regularly have all the necessary preventive examinations at the gynecologist. Just as important as the preventive care are the follow-up examinations after the illness. In the beginning, these are carried out every three months, later a six-monthly or annual cycle is sufficient. In addition to a cell smear, this follow-up check also includes an ultrasound examination of the vagina.
Aftercare
After the operation or radiation treatment, the patient should be examined every three months by the gynecologist or in the clinic for the first three years in order to detect a recurrence of the vaginal cancer (relapse) at an early stage. In a detailed discussion, the doctor gets an idea of the general condition of the patient and any complaints, during the subsequent gynecological examination, the vaginal mucosa is inspected with a special microscope and a sample (PAP smear) is taken.
This is examined in the laboratory for cell changes that could indicate a relapse. In addition, the doctor performs a vaginal ultrasound, with the help of which he can assess the vagina, uterus, ovaries and urinary bladder.If the doctor notices changes, he will order computed tomography (CT) or magnetic resonance imaging (MRI) to rule out metastases. Since recurrences are relatively common in vaginal cancer, it is extremely important to keep close follow-up appointments.
Even between the agreed examinations, the patient should see a doctor immediately if she notices bleeding, discharge or other changes in the vaginal area. Aftercare also includes psychological support for those affected after cancer treatment. Cancer counseling centers, self-help groups and resident therapists can help the patient and their relatives to process the disease and to cope with any problems that arise. In some cases, an inpatient spa stay can be useful.
You can do that yourself
Self-help that enables the disease to cure is not possible with vaginal cancer. Rather, it has to be about knowing possible symptoms of disc cancer on the one hand. The earlier it is recognized that a carcinoma has formed, the more favorable the prognosis. Regular self-examination in everyday life therefore makes an active contribution to prevention.
Even after a treatment, all follow-up appointments should be kept regularly. This is the only way to ensure that no metastases have occurred. Even if the disease cannot be cured primarily through self-help, affected women can improve their quality of life through their own efforts. In addition to general measures such as relaxation techniques, medication and ointments can also help reduce physical pain.
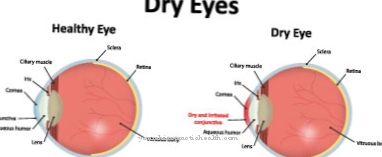
Many women suffer from a dry vagina after having a disc cancer removed, which can itch and burn in everyday life. Moisturizing ointments can often achieve a very great effect here, making the annoying but sometimes very agonizing side effects of the treatment bearable. Moisturizers for the vagina are now available over the counter from pharmacies. Cancer patients should, however, discuss all ointments and medications used in the vagina with their doctor.


.jpg)
.jpg)


















.jpg)



