The Bursitis, also as Bursitis is an inflammatory process of the bursa that manifests itself through the typical signs of inflammation such as swelling, reddening, overheating and pain in the affected area.
What is bursitis?
.jpg)
© Henrie - stock.adobe.com
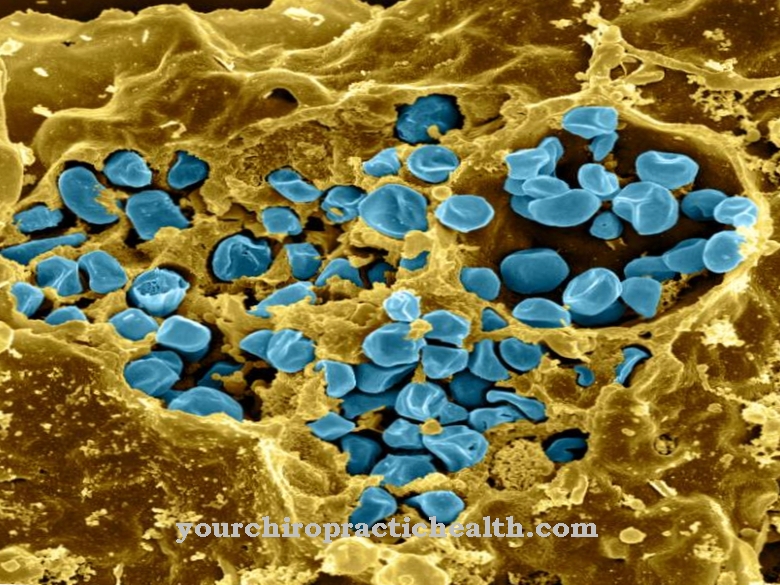
The bursa is anatomically precisely located on the joints and supplies them with the necessary synovial fluid.
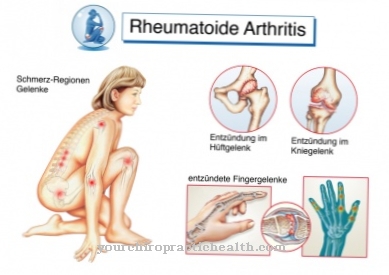
A Bursitis occurs mainly on the knee joint. The anterior front of the kneecap is affected by the disease-typical impairments associated with bursitis. For this reason, bursitis is a classic disease of the knee joint.
Bursitis can, however, also affect all joints that are particularly exposed to sometimes enormous mechanical pressure. For this reason, bursitis can often be diagnosed on the bursae of the joints of the elbow.
In addition, bursitis on the shoulder joint can even be associated with damage to the tendons and ligaments.
causes
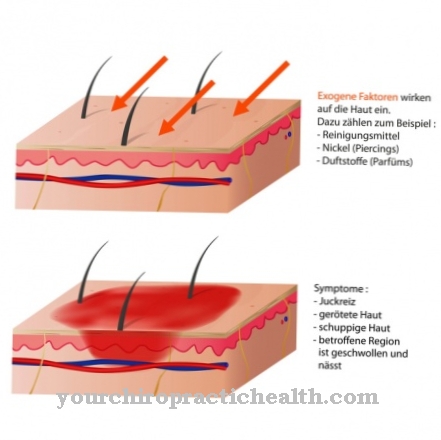
The causes one Bursitis are relatively easy to classify. Basically, all influences that can trigger a bursitis lead to the fact that the bursa in the joint is subject to inflammatory processes. This is because there may be too extreme pressure on the area. These can contribute to bursitis either through falls or monotonous and persistent unilateral movements of the joint.
Constant sitting, endurance sports such as jogging or tennis as well as special occupational activities place strong pressure loads on the bursa. These can react to these permanent excessive loads in the form of bursitis. From a physiological point of view, these effects result in microscopic injuries to the joints, which is the trigger for bursitis.
In addition, accidents, osteoarthritis or arthritis are also the causes of bursitis in the affected joint area.
Symptoms, ailments & signs
Bursitis is usually the result of excessive shoulder load. The pain often hits the person completely unprepared. Often the symptoms appear at night and it becomes impossible for the patient to lie on the shoulder. Due to the gradual progression and the initially minor discomfort, the bursitis is usually not taken seriously and thus dragged on.
However, the pain can become so severe that it may be necessary to see a doctor. The inflamed joint is red and swollen. The affected area hurts when touched. Due to the increased blood flow to the surrounding tissue, the affected area feels warm. The inflamed joint is restricted in its movement.
The bursitis is differently pronounced. If the symptoms are recognized early and taken seriously, the pain will improve after a few days. A postponed bursitis, on the other hand, can take a chronic course and pain and restricted mobility accompany the patient for months or years.
If the cause is not overwork but an infection, then pain, fever and a general feeling of illness also occur. Bursitis can occur on the shoulder, elbow, knee, or hip. The symptoms are identical in each case.
Course of disease
Typical for the Bursitis is that only with an advanced course and constantly existing causes permanently perceptible complaints occur. Chronic and acute bursitis are differentiated on the basis of the different courses.
An acute bursitis can develop into a chronic bursitis if the condition is untreated and further exposure to the trigger. Depending on the affected joints, bursitis initially leads to reddening, an increase in warmth and swelling, which are accompanied by pain and more or less severe restrictions on mobility.
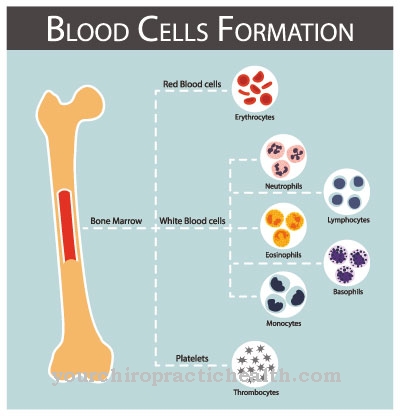
Synovial fluid collects in the bursa, which increases the size of the skin around the joints when touching the bursitis and makes it feel wobbly and doughy. After the bursa has been punctured, a liquid emerges that is called a secretion and resembles water in the case of bursitis (bursitis). If a strong mechanical impact on the joint has caused bursitis, then this fluid is stained with blood.
Complications
In the worst case, an untreated bursitis can cause blood poisoning.Usually, however, there are no or only slight complications - inflammation and injuries to the bursa, for example. The restricted movement can occasionally lead to malpositions. The inflammation can also spread to other regions of the body or even develop into a chronic disease.
The mostly severe pain generally represents a considerable physical and psychological burden for the person concerned. If the illness lasts for a long time, the complaints have a grueling effect and can subsequently also cause psychological illnesses or exacerbate existing ailments. When treating bursitis, undesirable complications can also arise.
An operation rarely leads to symptoms such as bleeding, secondary bleeding, wound healing disorders and scars. Injuries to nerves, tendons, muscles and ligaments are also rare, but cannot be ruled out. In addition, allergic reactions to the agents and materials used can occur.
Resting can lead to medium-term muscle weakness and thus to restricted movement of the joints. The risk of developing blood clots is also slightly increased. Prescribed medication can cause side effects and interactions and trigger allergic reactions.
When should you go to the doctor?
If there is pain and redness in the area of the bursa, there may be bursitis. A visit to the doctor is recommended if the symptoms of inflammation get worse and have not disappeared after three to four days at the latest. If there are other typical symptoms, such as signs of fever or restricted mobility in the knee, it is best to consult your doctor directly. The risk groups include people with rheumatic diseases and patients with tuberculosis, gonorrhea or other infectious diseases. Those affected should inform the responsible doctor if the mentioned symptoms are noticed.
The condition often occurs after an injury. If pathogens get into the tissue through a wound, inflammation and the symptoms mentioned occur. At this point at the latest, a visit to the family doctor or an orthopedic surgeon makes sense. Other contacts are the internist or a sports doctor. In the event of recurring complaints, a more detailed examination in a specialist clinic is useful. Those affected should also consult their doctor during treatment and inform them of any unusual symptoms. Antibiotics, in particular, can under certain circumstances cause further changes and side effects that need to be clarified.
Treatment & Therapy
To the Bursitis To be able to treat efficiently, conventional medicine regularly recommends conservative and surgical therapy. Various drugs are used in particular within the conservative treatments of bursitis. These drugs are intended to relieve both the inflammatory processes of bursitis itself and the annoying symptoms.
The cooling of the affected joint and the temporary restriction of movement as well as effective pain medication, anti-rheumatic and anti-inflammatory medicinal substances support the therapy in the case of bursitis. If the bursitis is caused by bacteria, antibiotics are given. If the painful and inflammatory processes are contained to a certain extent, then as a follow-up treatment for bursitis (bursitis), physiotherapeutic or physiotherapeutic care can restore the mobility of the joint.
In addition, ultrasound-assisted therapy is also considered effective. If the individual methods do not help, then the last step can be the surgical treatment of the bursitis. This is based on removing the inflamed bursa under local anesthesia. For quick healing after the procedure, immobilization with a fixation bandage or bandage is performed.
You can find your medication here
➔ Medicines against swellingprevention
Basically, a Bursitis can then be avoided if, as it were, all movements or postures that put stress on the joint and overstrain the joint are reduced. This mainly concerns the effects of strong pressure and movements that are carried out under the constant influence of forces that create friction in the joint. Hard falls to be expected should be prevented by appropriate protective elements in order to prevent bursitis.
Aftercare
In the worst case, an untreated bursitis can cause blood poisoning. Usually, however, there are no or only slight complications - inflammation and injuries to the bursa, for example. The restricted movement can occasionally lead to malpositions. The inflammation can also spread to other regions of the body or even develop into a chronic disease.
The mostly severe pain generally represents a considerable physical and psychological burden for the person concerned. If the illness lasts for a long time, the complaints have a grueling effect and can subsequently also cause psychological illnesses or exacerbate existing ailments. When treating bursitis, undesirable complications can also arise.
An operation rarely leads to symptoms such as bleeding, secondary bleeding, wound healing disorders and scars. Injuries to nerves, tendons, muscles and ligaments are also rare, but cannot be ruled out. In addition, allergic reactions to the agents and materials used can occur.
Resting can lead to medium-term muscle weakness and thus to restricted movement of the joints. The risk of developing blood clots is also slightly increased. Prescribed medication can cause side effects and interactions and trigger allergic reactions.
You can do that yourself
Throbbing pain, redness and swelling are the classic signs of bursitis, the appearance of which can also be alleviated by self-help. Going to the doctor is often not even necessary, for example if an athlete has had multiple experiences with the disease and knows how to treat it. As with many other inflammatory diseases, cooling is a tool that can often be used to manage the symptoms of bursitis well.
It is important that the ice is not applied directly to the affected area in order to exclude irritation of the skin. Ice cubes, for example, can be placed in a washcloth, which is then placed on top if no ice is available in the form of a classic cold pack. Cooling should be moderate anyway. If you work too hard with cold, the tissue may react with increased blood flow, which is rather counterproductive in the case of inflammation. Ice is therefore a suitable means in acute cases and pain, but not useful for long-term use.
Rest is also an important factor in bursitis. This means, for example, that kneeling should be avoided if the inflammation is manifested in the knee. Exposure to heat, such as hot baths, is also not advisable, at least in the acute stage. Athletes wait for the next training session and competition until the inflammation has subsided.















.jpg)