Thrombolysis softens a thrombus with the help of medication (fibrinolytics). However, this procedure is only possible with small and fresh thrombi. The synonym for thrombolysis is Lysis therapy. The medical specialties for thrombolysis are internal medicine, neurosurgery and cardiology.
What is thrombolysis?

A pulmonary embolism, a stroke or a heart attack can trigger thrombi due to blocked blood vessels. These blood clots obstruct the regular flow of blood in the body. One consequence of the thrombus is a deficient supply of blood and oxygen to the cardiovascular system. Cell death and tissue damage release activators that lead to fibrin formation via complex reactions.
This can result in both vascular occlusions and traumatic lesions that trigger bleeding. Thrombolysis is a physiological mechanism that removes obstacles to disturbance in the affected organs by breaking up the blood clot. The thrombolysis takes place by means of tissue-specific plasminogen activators. In order to prevent serious and life-threatening damage to the affected organs and the general state of health, these thrombi must be dissolved as soon as possible.
To do this, doctors administer medication to the affected patient as part of a drug therapy known as thrombolysis. The physicians introduce various drugs systemically into the patient's body by infusion via the bloodstream or locally at the thrombus. These drugs contain enzymes that cause certain reactions in the patient's body cells and release active substances that activate specific endogenous enzymes.
Function, effect & goals
Strokes, pulmonary embolisms and heart attacks are the result of blocked blood vessels. These are caused by the clumping of the blood. This process is triggered by the protein fibrin. The precursor to fibrin is fibrinogen, which is constantly in the bloodstream. This endogenous substance in itself is harmless until it is activated, for example by damage to a vessel wall, and turns into fibrin.
The fibrin now forms a fine and dense network that catches blood cells and converts them into a plug that eventually clogs the blood vessels of the affected organs and triggers a thrombus. In cardiology, thrombolysis is now the "gold standard". This drug therapy is also known under the short term "lysis". To treat a myocardial infarction caused by a thrombus, cardiologists use three active ingredients: 1) the protein streptokinase produced by the streptococcus bacteria, 2) the body's own protein urokinase, which is found in the urine and tissue, 3) the genetically produced substance tissue plasminogen activator ( tPA), which is similar to an endogenous anti-coagulant.
The tPA substance is used in particular in the thrombolysis of stroke patients. The Tissue Plasminogen Activator is genetically engineered. This is why the abbreviation rtPA is often used, with the first letter standing for recombinant (genetic engineering). The human body regularly produces tPA in very small quantities, which acts as the body's own police force in the fight against the effects of harmful substances. As soon as there is a risk of blood clotting or clumping, the tPA ensures that these undesirable blood symptoms are resolved in healthy people.
If, in the event of a heart attack or a stroke, a larger blood clot forms with the risk of blood clumping, the rtPA injected by means of thrombolysis activates the body's own substance plasminogen. This attacks the fibrogenic network and the resulting thrombus and dissolves it. Lysis is carried out in two ways. In local therapy, the rtPA is brought as close as possible to the clot in the bloodstream.
The rtPA is systemically distributed throughout the body through an infusion. Which of the two methods the medical professionals use depends on the extent to which the thrombus is accessible. Lysis is also the first acute measure in the case of a stroke, because if used successfully, patients recover from the consequences more quickly within a time window of three to four hours than patients in whom this drug therapy was not carried out. The time window for thrombolysis is four hours in order to rule out life-threatening consequential damage. This shows that the principle of “time equals brain” is once again justified.
To successfully carry out thrombolysis, every quarter of an hour counts. Every fifteen minutes lost increases the likelihood that patients will be discharged home healthy by three percent. The earlier the thrombolysis is carried out successfully, the less patients suffer from the consequences of a cerebral haemorrhage, a cardiac thrombus or a pulmonary embolism. The death rate drops by four percent (American NINDS study on thrombolysis, American medical journal JAMA (2013; 309: 2480-2488).
Risks, side effects & dangers
Thrombolysis is only an instrument for acute emergency situations. It is unsuitable for regular use because the use of such drugs is associated with a high risk of bleeding. Despite these treatment dangers, thrombolysis has gained acceptance as an emergency measure in recent years after large-scale studies have shown that the benefits of this therapy far outweigh the disadvantages associated with the risks.
There are some contraindications to lysis. It must not be used in case of allergies to the drugs used. If the symptoms were more than three hours ago or if they cannot be clearly assigned, the lysis must never be used. Further contraindications are a stroke within the last three months and a heart attack within the last three weeks. For example, there is a great risk of bleeding when taking blood-clotting medication in cardiac patients. Further contraindications are too high or too low blood sugar levels and high blood pressure.
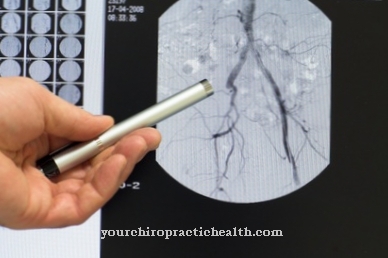
Before thrombolysis is used, if a stroke is suspected, computed tomography must be performed to determine whether this is due to an ischemic insult, or reduced blood flow. Lysis therapy must be started within the first three hours after symptoms appear. During this time, the patient is taken to the hospital's stroke unit, where the option of a cranial emergency CT scan (image of the skull) is always available.
This therapy is carried out exclusively under the supervision of an experienced doctor in neurological intensive care medicine. The performing radiologist must be qualified to evaluate cranial computed tomography in the early phase of the ischemic insult. In addition, interdisciplinary collaboration with a nearby neurosurgical center must be guaranteed.
















.jpg)

.jpg)


.jpg)