At Tinea or. Dermatophytoses These are infectious diseases that are caused by certain fungi and primarily affect the skin, but also hair, as well as the fingernails and toenails.
What is tinea?
.jpg)
© phanasitti - stock.adobe.com
The ancient Greek name Dermatophytosis derives from the terms for "skin" (derma) and "plant" (phyton). The Latin name Tinea ("Woodworm") is also common.
Dermatophytosis can occur in different parts of the body. The clinical picture can be very different depending on the type of fungus and body region - there is often reddening, itching, scales and blisters. The best known is probably tinea pedis, the athlete's foot.
About every tenth to fifth person will develop dermatophytosis in the course of their life; it is therefore the most common dermatological disease and one of the most common infectious diseases.
causes
Dermatophytosis is triggered by so-called thread fungi. These are thread-like, unicellular fungi that settle in the hair, nails and skin of humans and animals. A distinction is made between microspores, trichophytes and epidermophytes.
They are transmitted from the outside to humans - either from one person to the next, via contaminated surfaces (as often happens with athlete's foot) or through close contact with animals, especially rodents, rabbits and cats.
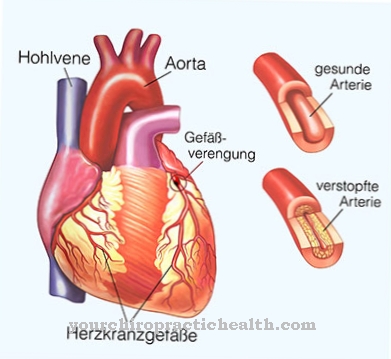
People with a weakened immune system and people suffering from diabetes mellitus, circulatory disorders of the skin or overweight are significantly more likely to be affected.
Typical symptoms and complaints
- Ring braid
- Reddening of the skin
- Itching
- Abscesses
Diagnosis & course
Dermatologists differentiate between superficial and deeper Dermatophytosis. The superficial form (tinea superficialis) usually manifests itself as redness and itching on limited skin regions, which are often ring-shaped and surrounded by a darker edge. Sometimes it comes to hair loss or a thinning of the hair growth in the affected region.
With deeper dermatophytosis (tinea profunda), inflammation occurs, which can also be accompanied by the formation of pus and crusts. It is found primarily in the area of the scalp and beard, as the pathogens penetrate deeper into the skin along the hair roots. A rapid test for dermatophytoses is possible using the so-called Wood light. This is a black light lamp, in the light of which affected skin regions appear yellow-greenish.
In the diagnosis of dermatophytosis, it is crucial to precisely determine the causative fungus in order to enable effective treatment. For this purpose, the doctor takes a sample of the affected tissue. By creating a mushroom culture, information about the exact pathogen strain can be obtained.
Complications
Dermatophyte infections are not uncommon and, if treated appropriately, usually heal without complications. Complications are to be expected in particular if the disorder is not taken seriously and is therefore not treated or if the patient's immune system is severely attacked. In these cases, tinea corporis, for example, can develop.
This infection affects the entire body, including the limbs, and can be very itchy. In addition, deeper dermatophytoses (tinea profunda) can develop. These mainly affect the head and other hairy regions. In men, the part of the face that also shows beard hair is particularly affected.
Tinea profunda can be accompanied by purulent inflammation, which can be confused with purulent pustules, similar to that of an acne disease. Deeper dermatophytoses in the head area can also lead to the scalp hair falling out, whereby only individual areas of the skull can be thinned or the hair can break off even under low stress.
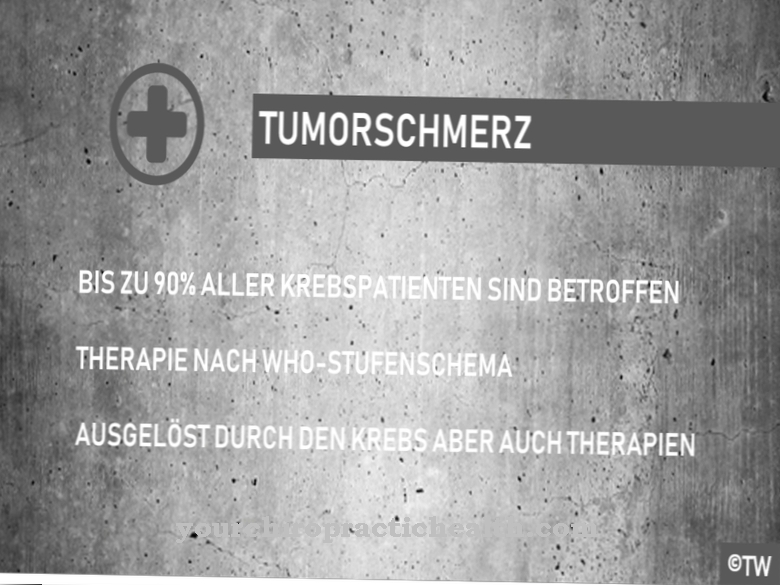
In patients whose immune system is not fully functional, especially children, people who suffer from diabetes mellitus or are infected with HIV, there is also the risk that the fungal infection will become severe and affect the internal organs.
The treatment is often made more difficult by the fact that fungal spores can be transmitted very easily and therefore there is very frequent reciprocal infection between members of a household, which can also affect pets.
When should you go to the doctor?
Dermatophytosis can be treated at home with over-the-counter treatments. Fungicidal ointments and creams for application to the skin make the fungus disappear again within days or weeks. However, a visit to the doctor should be considered if the person concerned suffers from dermatophytosis for the first time and may not be able to determine where the redness on the skin is coming from. Reddened areas of skin can have many different causes that the layman cannot tell apart. Differential diagnoses include a contact allergy, mechanical irritation or a reaction to chemical substances such as the wrong care product.
The doctor often recognizes at first glance whether it is a dermatophytosis or not and can then carry out appropriate examinations of the reddened skin to confirm the diagnosis. Then nothing speaks against the patient treating the dermatophytosis himself at home. Since tinea often occurs in connection with existing diseases such as diabetes, those affected treat it themselves without a doctor's visit, as they already know what the redness is. However, if it does not go away within a few days, the doctor should still examine the suspected dermatophytosis. The redness may be caused by another cause or the drug may need to be changed. It is also conceivable that the dose of the over-the-counter ointments is insufficient for stubborn dermatophytosis.
Treatment & Therapy
Heal in healthy people Dermatophytoses partly also untreated again; however, without medical therapy it often becomes chronic. Treatment with ointments containing benzoic acid, for example, is often sufficient for mild forms.
With reliable evidence of dermatophytosis, antimycotics, specialized agents against fungal attack, are used. These can either be applied to the affected area of the body in the form of creams, ointments or tinctures or - in severe cases - they can also be administered in tablet form.
During therapy, care should be taken to change laundry and towels regularly and to wash them at at least 60 degrees to avoid re-infection. The affected parts of the body should not be touched so as not to drag the dermatophytes away.
If these points are observed, the treatment of dermatophythosis is generally unproblematic and complete healing can be expected. Due to the skin's ability to regenerate, there are usually no visible traces left and even broken hair usually grows back completely.
You can find your medication here
➔ Medicines against redness and eczemaprevention
There have already been efforts in medical research to have a vaccine against the infestation Dermatophytes to develop; However, this was not suitable for the masses because of strong side effects.
The most effective prevention is to avoid contact with potentially infected surfaces. This includes wearing suitable shoes in public swimming pools, communal showers and hostels. However, even in private settings, care should be taken to ensure that towels and clothing are not shared by several people.
Dermatophytes thrive in a warm and humid climate, so feet and skin folds should always be dried thoroughly; Breathable, airy clothing is also an advantage in this context. The usual hygiene precautions must also be observed when dealing with pets and farm animals.
You can do that yourself
Patients with tinea (dermatophytosis) initially focus on treating the disease with medication. Because self-healing can take a long time.
Those affected regularly use the prescribed drugs, usually antimycotics to be applied to the skin, in the prescribed dose. They observe the reaction of the diseased skin and see a doctor in the event of side effects or delayed healing. Since tinea (dermatophytosis) is often accompanied by severe itching in the affected areas, patients must learn to resist the itching and not scratch the areas of the skin affected by the fungus. Touching the diseased skin areas is generally rather detrimental to healing and often exacerbates the symptoms. In addition to aggravating the itching from scratching, there is also a risk that the fungus can spread to other parts of the body.
During the illness, clothing should not lie close to the skin and allow sweat to evaporate well. Natural fibers and hypoallergenic textiles that are cut as wide as possible and allow good air circulation are therefore well suited.
After all, hygiene plays an extremely important role during the illness. Patients with ringworm avoid going to public swimming pools and saunas.

.jpg)

















.jpg)



