Toothache that suddenly stops? Tooth discoloration, no cold stimulus, but bite sensitivity? Typical signs for a dead tooth speak. It is important that the dead tooth is not ignored, but treated by a dentist. This is the only way to save it from extraction.
What is a dead tooth?

© Henrie - stock.adobe.com
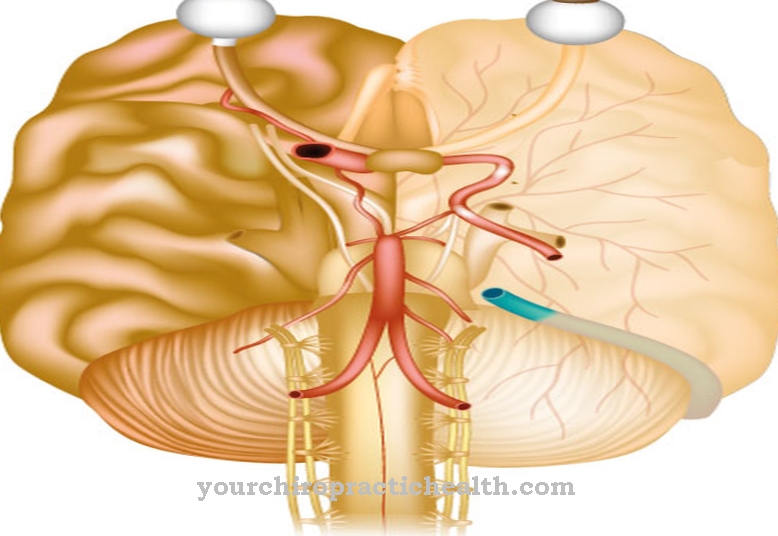
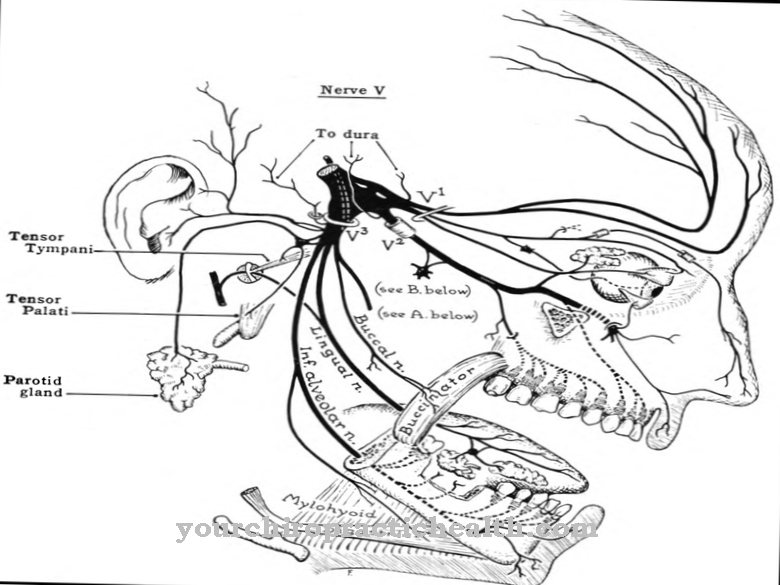
If the dentist finds holes in the tooth that are too deep and caries that is very advanced, there are hardly any options left to actively ensure that the tooth remains alive. The tooth - or rather the pulp - subsequently dies. The pulp is a bundle of blood vessels and nerves that supply the tooth.
A dead tooth but does not have to drop out on the spot; sometimes it can go unnoticed for a long time. On the one hand, because a tooth that has no nerve does not cause any discomfort and, on the other hand, because the tooth enamel remains stable even if there is no blood supply.
However, the tooth becomes discolored; over time it becomes dark. Sometimes the person concerned complains of a bite sensitivity and constant breaking off of tooth substance. In the worst case, there is swelling and severe pain.
causes
As a rule, an inflammation of the pulp, the so-called pulpitis, is responsible for the death of the tissue. Pulpitis occurs when pathogens - due to the deep holes caused by caries - reach the tooth nerve. Pulpitis causes extreme pain, but on the other hand it can also proceed without discomfort.
If the tooth nerve is inflamed, this subsequently destroys the entire pulp. If the person concerned complains of severe toothache, which, however, disappears on its own after a few days, no spontaneous healing has occurred, but the tooth nerve has died. Acute pulpitis has developed into chronic pulpitis. For this reason, it is important to see a dentist in good time. In rare cases there is direct damage to the pulp. Occasionally, accidents in which the tooth is knocked out or breaks can cause direct damage to the pulp.
Symptoms, ailments & signs
A dead tooth doesn't necessarily have to cause pain. A typical sign that a tooth has already died is insensitivity to cold. The affected person visually notices a dark discoloration. Sometimes there is also severe toothache; If the toothache subsides after a few days and disappears so that there is suddenly no pain, the tooth has died.
Diagnosis & course of disease
Before the treatment, the doctor checks whether the tooth is vital or dead. He sprays a cotton ball with the cold spray, which he then places on the tooth. Sometimes, however, a short puff of air from a water-air pistol is enough to determine whether the tooth has died or not.
If the patient perceives the cold stimulus, it is a positive vitality test - the tooth is alive. In the event of a negative vitality test, the dentist must assume that the tooth has already died. However, further examinations must be carried out in this regard, as fillings or crowns can impair the vitality test.
Using percussion testing, the doctor can also test whether the tooth has already died or not. If the patient reacts to knocking directly on the tooth, there is inflammation in the jawbone. The doctor speaks of the root tip inflammation.
The patient usually suffers from jaw pain; the dead tooth does not cause pain. If in doubt, the dentist can have an X-ray taken.In the picture, the doctor recognizes a circular change that has arisen directly at the tip of the root and suggests that a tip inflammation has occurred.
The dead pulp is of course the perfect breeding ground for countless bacteria. Those come directly from the oral cavity and can easily migrate into the tooth. The bacteria also have an easier time when tooth decay has already formed. Due to the fact that bacteria enter, the dead tissue begins to rot.
Aggressive inflammation develops, so-called gangrene, which is mainly noticeable by an extremely foul odor. The pathogens that can be found in the whole jaw cause inflammation that is not harmless. If the inflammation breaks through, i.e. if it affects the surrounding tissue next to the tip of the root, an abscess occurs. A fact that can be recognized immediately by the "big cheek".
Complications
A dead tooth does not necessarily have to be extracted, but if it is not treated by a dentist, it can be problematic because bacteria from the oral cavity penetrate the dead pulp and cause the tissue to rot and cause inflammation. Mostly it can be recognized by a putrid bad breath.
Often the tooth starts to throb and becomes very sensitive to pressure because the pressure cannot escape due to the putrefactive gases. It is dangerous if the inflammation is not treated properly because it can spread through the entire jaw via the tip of the root. When pus flows into the adjacent tissue, the cheek becomes thick, as the vernacular says.
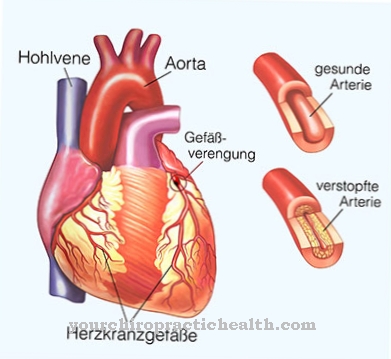
The bacteria can enter the bloodstream through the jaw and cause health problems in other parts of the body, including myocarditis, which at first glance would not be seen in connection with the dead tooth. The tricky thing is that dead teeth don't always make themselves felt as pain.
Often they simply die and the bacteria can multiply unhindered over a long period of time without the affected person noticing. It is therefore important to treat such a dead tooth early so that it does not become a bacterial focus.
When should you go to the doctor?
A dead tooth behaves like any other dead tissue in the body over the long term. Therefore, the dentist should be consulted at an early stage, who will remove dangerous components of the tooth and try to preserve it as much as possible and to make it look like a healthy tooth with suitable dentures. The person affected will probably not notice that a tooth has died at first. Only over time will pain and then visual changes in the tooth appear. Since these are characteristic signs of dead teeth, now is the right time to see a doctor.
The family doctor can help out with painkillers for a short time in acute pain if the first symptoms occur on weekends or holidays. Even then, however, it makes more sense to seek short-term treatment in an emergency dental practice, since pain medication alone does not solve the problem of the dead tooth.
If the dentist were not to be seen, the tooth would continue to decay, even if dental care continued as usual. The affected person could no longer prevent bacteria from spreading to other surrounding teeth and starting to destroy their tooth enamel if that had not already happened. The immediate visit to the dentist is also important to protect teeth that are still healthy.
Treatment & Therapy
A dead tooth must be treated by the dentist. If the dead tooth is ignored, chronic inflammation ensues. In the end, the doctor can only remove the tooth. If the patient reacts in time, the dentist can try to somehow save the tooth.
He performs a root canal treatment. The root canal is cleaned and then closed with a filling. However, if the dentist can no longer save the tooth because it is already too brittle, too loose or permanently infected, he can only remove it. An extraction follows. The resulting tooth gap can then be closed with a bridge, a removable denture or an implant.
You can find your medication here
➔ Toothache medicationprevention
A dead tooth can definitely be prevented. Regular dental care, oral hygiene and check-ups at the dentist - all factors that prevent tooth decay from forming. Toothache sufferers should see a dentist as soon as possible; Sometimes one filling is enough to prevent further problems.
Aftercare
After treating a dead tooth, follow-up care is of great importance. Regular visits to the dentist are necessary as possible infections can be detected and treated early after a tooth has been removed. If the dead tooth is preserved, it must be checked regularly, as problems and loss of function are more likely in the long term than with healthy teeth.
Basically, the person affected should have their teeth cleaned regularly by a professional. The dentist is best able to decide on the frequency of these cleanings. In addition, the patient should ensure that their teeth are cleaned regularly and thoroughly. This includes brushing your teeth with toothpaste and toothbrush after meals, as well as using cleansing mouthwash and floss.
These measures are also a general prevention against tooth decay and the associated damage to the teeth. If the dead tooth is preserved, pain sensations can still occur. The tooth itself is dead, but it is still surrounded by nerves that can emit a pain signal under strong pressure. In this case, the person concerned should see a dentist as soon as possible.
You can do that yourself
With a dead tooth, working with a doctor is very important. Otherwise, complications and secondary diseases can arise in everyday life. Dental hygiene is by no means neglected just because the tooth has died. Rather, it has to be optimized and adapted to the needs of the organism.
The dead tooth should be taken into account when cleaning the mouth, tongue and teeth if possible after each meal. It must not be left out when cleaning the teeth several times a day, otherwise bacteria or other germs will form. These can multiply and spread within a short time. The person affected should therefore use dental floss, mouthwashes or other care products in addition to toothpaste.
Depending on the cause of the dead tooth, there is an additional risk of spreading or new development of symptoms without medical care. If possible, a tooth rescue should be initiated or a denture will be needed. These processes cannot be carried out independently.
To strengthen the organism, it needs a healthy immune system. In order to cope better with the treatment and to promote the healing process, it is therefore important to ensure that the body's own defense system is adequately developed. When eating, the food should not be too firm to avoid chipping teeth.


.jpg)

.jpg)