The American doctor and microbiologist Robert Guthrie led the 1963 Dry blood test, the Guthrie test, which was used to diagnose the metabolic disease phenylkenonuria (inability to break down the amino acid phenylalanine because an important enzyme in the body is missing) in newborns.
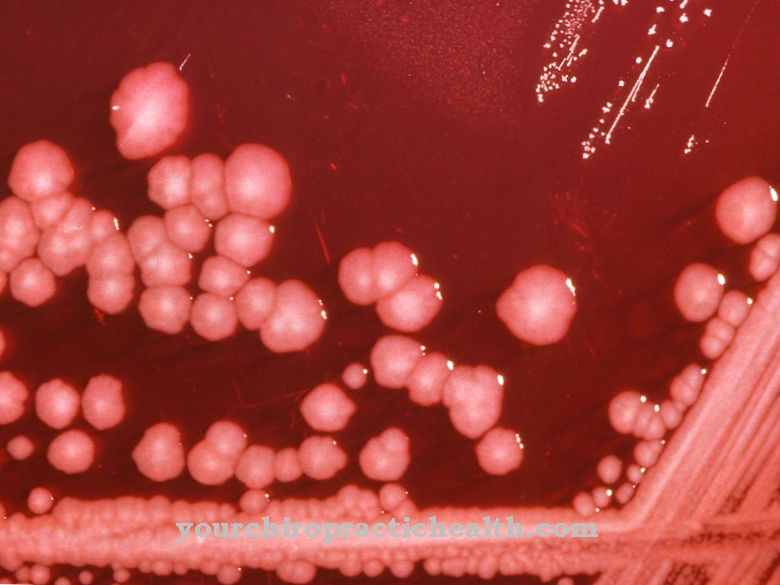
This screening method is still used worldwide today in which a few drops of blood are dripped onto a special filter paper of newborns. After the blood has dried, the filter paper is placed on a nutrient-containing agar plate without phenylalanine and a certain type of bacteria is added.
These special bacteria can only multiply if there is a lot of phenylalanine in the dried blood drop. This is used to determine whether a newborn baby has the congenital metabolic disease and therefore needs a special diet. Recognized at an early stage, these newborns can grow up normally with a strict phenylalanine-free diet without the risk of mental malformations.
What is the dry blood test?

In later years, further factors in the blood for congenital metabolic diseases were recognized, so that nowadays routine screening of newborns between the 36th and 72nd hours of life for certain metabolic disorders with the dried blot spot (DBS) test is standard.
To catch a drop of blood with a special filter paper, the newborn only needs to be piked briefly on the heel. The dried filter papers are sent to selected special laboratories, where they are now tested for more than 30 metabolic diseases using complicated but efficient analysis methods. Doctors, and thus parents, receive the test results within hours or a few days. For ethical reasons, only diseases that are diagnosed at an early stage and are treatable are recorded as part of the newborn screening.
Nowadays, newborn screening with the dry blood test is mandatory in many countries, but not in Germany. Nevertheless, this screening process for newborns is also used by many parents in this country and financed by the health insurance companies.
Function, effect & goals
The simplicity of taking blood for the dry blood test led to the fact that this examination method was also established for older children with other diseases, in order to spare them the painful need to take venous blood with the needle.Nowadays, the DBS method is used in many areas of in vitro diagnostics (examinations outside the body by taking blood, urine or saliva beforehand), including for adults.
A small prick in the finger is enough to drip enough blood onto the special filter paper. For example, the concentration of vitamin D in the blood is determined using the dry blood test. Low levels of vitamin D indicate certain conditions. Even if the patient is still symptom-free at the time of the examination, the attending physician can immediately initiate therapy.
For therapeutic drug monitoring, in which doctors need to know whether the dose of a prescribed drug is correctly set in the blood, dry blood tests are sometimes used. For the DBS procedure, the doctor can also give the patient the utensils necessary for finger pricks and blood collection to take home. In this way, it can drip drops of blood onto the corresponding filter papers over a longer period of time and allow them to dry. He then brings this with him to the next doctor's visit, or sends it directly to the designated laboratory. In this way it is also determined whether a patient is taking his vital medication, such as anti-epileptic drugs, correctly.
In this context, the individual dose setting of immunosuppressants is a particular focus for the dry blood test. In order to set the correct concentration of medication after an organ transplant, patients often have to have their blood drawn at very short intervals. This is another advantage of the DBS method, as the already weakened patient is only slightly stressed when taking the blood.
It is also practical that usually only a very small piece of the blood dried on the filter paper is required for the laboratory test and therefore different tests can be carried out using the same blood drop. The "blood cards" can be stored in a clean, dark and cool place for many years. If desired, it can also be checked after a long period of time whether or not a certain parameter in the blood has already been suspicious. In addition, this type of blood collection ensures more safety for the medical staff against puncture injuries (possible transmission of infections is thus further minimized).
Even laboratory staff benefit from this type of examination, as it saves time and consumables when pretreating the blood sample. Whole blood in tubes must be pretreated in a complex process, which is more time-consuming and expensive.
Risks, side effects & dangers
However, this type of blood collection also carries risks for later examination in the laboratory. In particular, if the filter papers are given to the patients at home, it cannot be ruled out that they may use the utensils improperly and thus the respective filter paper will become unusable.
Furthermore, bacterial contamination or other dirt lead to unusable test results. Scientific studies show that certain parameters such as for some hormones, test results can vary widely between venous blood and dry blood tests. The reason for this is, among other things, the different amount of hematocrit (proportion of erythrocytes in the volume of the blood) depending on the blood collection method.
Therefore, many clinical studies are running with dry blood tests to improve their reliability for certain parameters. If necessary, the analysis methods are adjusted or, if necessary, blood from the vein is recommended. There are now dry blood tests for certain pets and farm animals.





.jpg)










.jpg)

.jpg)