The Tunica intima is the three-layer inner layer of the lymph and blood vessels. In addition to an optimal lymph and blood flow, this layer creates a barrier for the diffusion of various blood and lymph components. Tears in the inner tunica intima are a life-threatening phenomenon, especially in the aorta.
What is the tunica intima?
Human blood vessels are made up of different layers. The innermost layer is called the tunica intima. The term comes from Latin and literally means something like "inner garment". The tunica intima not only ensures an optimal flow of lymph and blood fluid, but also represents a selectively permeable barrier for dissolved components of the blood.
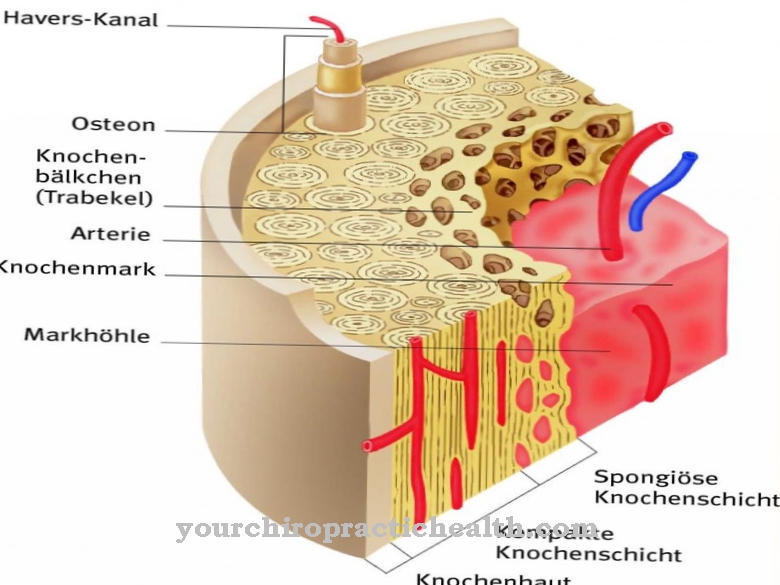
This means that various blood components are allowed to enter through the barrier, while other molecules are kept away from the interior of the vessels by the barrier. The tunica intima itself is made up of several layers, with its individual layers fulfilling different tasks. All blood and lymph vessels in the entire body are equipped with a three-layer tunica intima. The individual layers correspond to the endothelium, the subendothelium below and a fiber network with elastic properties. Viewed from the lumen, the tunica intima lies directly on the tunica media, i.e. the middle layer of the vessels.
Anatomy & structure
The tunica intima has an average thickness between seven and 140 µm, depending on the type of vessels. The vascular layer is often referred to as the inner layer of the blood and lymph vessels, but itself consists of a total of three layers. On closer inspection, it is actually not about "the inner layer", but about the "inner layers" of the vascular tissue.
The base layer of the tunica intima is the monocellular and smooth endothelium. This tissue is in direct contact with the contents of the vessels, above all with blood. Endothelial cells are always flattened and polygonal in shape. The nucleus of the endothelial cells is arched into the lumen of the vessels. In addition to the endothelial layer, the tunica intima has a subendothelial layer. As the name suggests, this layer lies beneath the endothelium. A thin basement membrane made of loose connective tissue lies between the endothelium and the subendothelium. This layer is an elastically fenced tissue layer that carries elastic fiber networks, contains fibroblasts and has smooth muscle fibers.
Function & tasks
One of the main tasks of the tunica intima is to create the optimal flow. The inner surface of the endothelial cells is extremely smooth. Since this layer of the tunica intima is in direct contact with the blood, an ideal blood flow is guaranteed. The endothelial surface with the lumen-side alignment repels solid blood components. Erythrocytes or leukocytes can therefore not attach themselves to the vascular tissue.
In addition to these tasks, the endothelium takes on the function of a selectively permeable barrier for the dissolved blood components. Small-molecule blood components diffuse through the endothelium depending on the concentration gradient, while large-molecular components cannot diffuse. In addition, the endothelium of the vessels is able to release vasoconstrictive and vasodilatory substances. In this way, the vascular endothelium controls the state of tension in the smooth vascular muscles and in this way influences the blood pressure. The vasomodulatory substances of the endothelium include, for example, nitric oxide. In addition to the blood interaction of the vessels, the endothelium controls the interaction and communication with the surrounding tissues.
This communication and interaction includes the control of the vascular wall tone, the thrombus-inhibiting effect and the control of all processes of the exchange of substances. The endothelium is also relevant for blood clotting. Active ingredient precursors and active ingredients for coagulation are contained in the endothelium and act on the fibrinolytic coagulation system. For example, heparin sulfate and thrombomodulin inhibit blood clotting and prevent thrombus formation.
Diseases
Erythrocytes accumulate on damaged endothelium. This process characterizes inflammation, for example. The accumulation causes the endothelium to produce cell adhesion molecules that attract other cells to the plan and move them to adhere to the walls of the blood vessels. Apart from these disease processes, the tearing of the tunica intima is of particular pathological relevance. A tear in the layer causes the blood to wash away. A dissection occurs. Aortic dissection in particular should be emphasized in this context.
The phenomenon is also known as aneurysm dissecans aortae and is associated with a splitting of the wall layers within the main artery. The causal tear in the tunica intima leads to bleeding between the layers of blood vessels and causes sudden and severe pain. An aortic dissection is an acute risk to life. As a result of the phenomenon, the main artery can, for example, burst or at least cause circulatory disorders in individual organs. Apart from these disease processes, a minor injury to the tunica intima can also have serious consequences. All injuries to the inner vascular layer can cause intimal hyperplasia, for example.
The tissue layer of the inner vascular wall multiplies through exaggerated processes of cell division. In most cases, it is mainly the smooth muscle cells within the tunica media that are involved in cell growth. The processes are subject to stimulation by the platelet-derived growth factor. Platelets attach to the vascular injury.
Extracellular matrix such as collagen and elastin are produced in excess due to the influences and can result in a narrowing of the lumen or even a complete vascular occlusion. Atherosclerosis is also relevant as a disease in connection with the tunica intima, in which fat, thrombi, connective tissue and calcium are deposited on the inner endothelium of the vessels. Atherosclerosis promotes thrombus formation, strokes and heart attacks.


















.jpg)



