In the Type I allergy is a group of different allergic hypersensitivity reactions in the human body. The classification of the type is based on the classification of Coombs and Gell into four different types. According to current knowledge, this classification is immunologically outdated, but for didactic reasons it is still retained and taught in medicine.
What is Type I Allergy?
The Type I reaction is the "classic" of the allergic reaction, the "instant type", in which allergens such as pollen or animal hair trigger a release of messenger substances within seconds to minutes via binding to certain antibodies on so-called mast cells of the mucous membranes.
This leads to typical allergic symptoms such as swelling of the mucous membrane, the urge to sneeze, itching and reddening of the eyes, asthmatic attacks or, in the worst case, a drop in blood pressure and life-threatening anaphylactic shock reactions.
causes
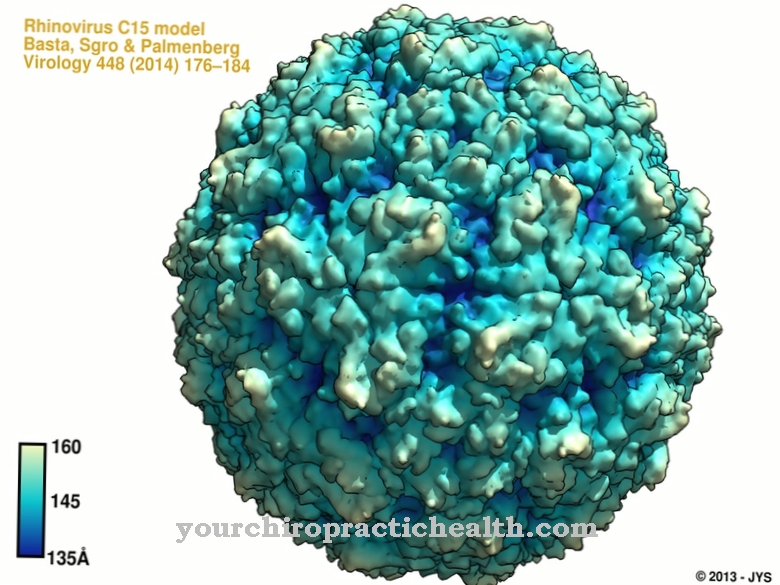
Such a reaction is usually triggered by large molecules such as pollen, protein, medication, contrast media or insect venom. Usually, the body's response to an antigen makes sense because it allows viruses and bacteria to be recognized and repelled as quickly as possible.
In the case of allergies, however, the body's defense strategy has gotten out of hand: the body reacts to substances that are harmless in themselves as if they were a pathogen. To do this, you first need to be sensitized: when you first come into contact with the antigen, nothing major happens. At the cellular level, however, the antigen is recognized as foreign, slowly processed, and the body builds mast cells into its mucous membranes, which only specialize in triggering an immediate defensive action the next time the same antigen appears.
If there is a second contact after such a sensitization, these specialized mast cells release massive and completely exaggerated messenger substances, which then trigger the symptoms described above. In addition to this immediate answer, the Type I reaction there is also a delayed response which begins after several hours, can last for days and consists of tissue infiltration with inflammatory cells.
Symptoms, ailments & signs
An allergy can trigger various complaints of varying intensity. These either extend to individual parts of the body or to the entire organism. When an allergy occurs, it usually belongs to type I. A good 90 percent of all cases can be attributed to it. Signs appear immediately, after a few minutes or hours.
The most common complaints affect the skin and the respiratory tract. The skin is red or a rash has formed. Wheals often appear. People start coughing. The swollen mucous membranes ensure that even shortness of breath can set in. Asthma attacks are possible.
The nose, which is also used for breathing, sheds liquid mucus. There is a constant urge to sneeze. The allergic reaction sometimes causes the eyes to redden. There is an uncontrollable flow of tears. Some patients even feel their eyes sting. All of the named symptoms represent a defensive reaction of the body.
In addition, general signs may accompany a type I allergy. As a result of the reaction, sufferers sometimes complain of sudden fatigue. Headaches and diarrhea can also occur. If the entire organism shows symptoms, caution is required. Anaphylactic shock is life threatening.
Diagnosis & course
The Type I allergy of the body can remain locally limited. This leads to reddening, swelling and the formation of wheals on the skin with itching. If the respiratory tract is affected, as is the case with pollen allergy (hay fever), the result is a runny nose, the urge to sneeze and the airways swell.
If the whole thing happens one floor below, an asthma attack can also be triggered by the will of the bronchi. A hay fever, for example, can get worse over the years and turn into asthma ("floor change").
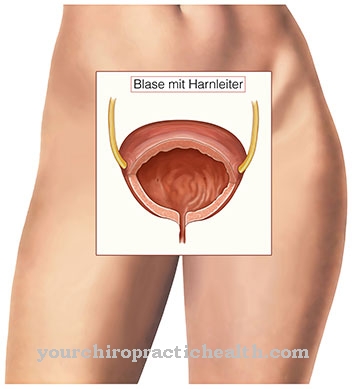
If the reaction does not take place locally, for example after systemic administration of medication or contrast agent, the type I reaction can also take place throughout the body and then primarily affects the bloodstream. Initiated by the released mediators, blood vessels are widened throughout the body, the blood sinks in the legs, is absent in the brain and the affected person becomes unconscious.
This severe reduction in blood pressure leads to a life-threatening lack of oxygen in the brain and internal organs and is known as "anaphylactic shock". It can also arise, for example, if you are stung by a wasp, have an allergic reaction and then pass out. Emergency medical treatment is then vital.
The doctor will usually determine the allergic cause of an emergency based on history. It is therefore important to be able to provide reasonable information about the circumstances under which a hay fever, reddening of the skin, an asthma attack or, in the worst case, fainting occurred.
Complications
Type I allergies, the most common type of allergy, are characterized by typical inflammatory reactions immediately after contact with the allergen. In most cases there are no complications. When the allergen contact is ended, the inflammatory reactions usually subside quickly. However, in a few cases these immune reactions can become so violent that life-threatening complications can occur.
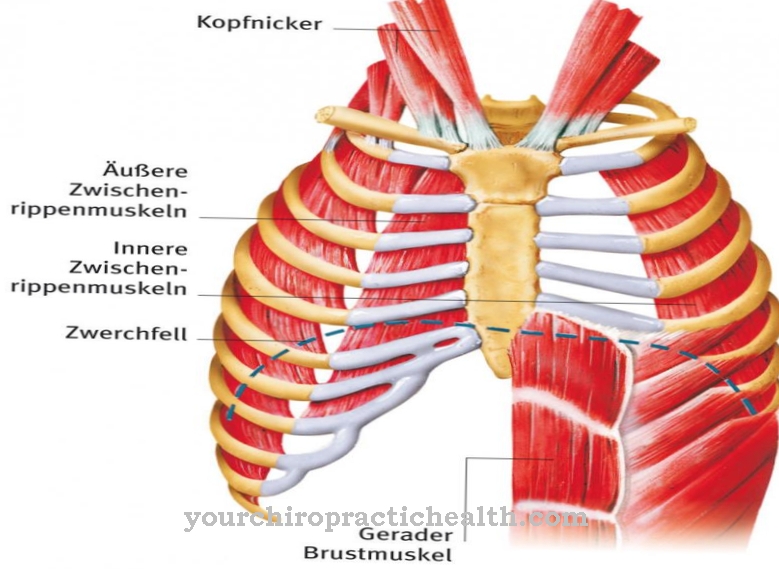
The main complications of type I allergy are allergic asthma and anaphylactic shock. Like other forms of asthma, allergic asthma can in extreme cases become a life-threatening emergency. Severe asthma is characterized by severe shortness of breath, inflated thorax, cyanosis (bluish discoloration of the lips due to lack of oxygen), exhaustion or even confusion. Coughing and racing heart always occur.
The shortness of breath can become so severe that the patient's life is in acute danger. Anaphylactic shock is always a life-threatening crisis that requires immediate treatment. It is a circulatory shock caused by massive vasodilation. The blood pressure drops sharply and the pulse can hardly be felt.
The heart rate increases extremely to compensate. Volume replacement therapy must be performed immediately to save life. Drug therapy can include the use of adrenaline. If possible, the triggering allergen should be removed immediately. In both allergic asthma and anaphylaxis, the symptoms quickly subside after the allergen contact is interrupted.
When should you go to the doctor?
The person concerned should always consult a doctor with a type I allergy. Since this disease cannot cure independently and the symptoms usually significantly limit the life of the person affected, the disease must always be checked by a doctor. A complete cure is not always possible, but the symptoms can be significantly alleviated. As a rule, the doctor should be contacted if the person concerned suffers from severely reddened skin or if there is a severe rash on the skin. These complaints usually occur when the person concerned comes into contact with a certain substance or ingests it. Burning eyes or breathing difficulties can also indicate type I allergy. Many patients also suffer from diarrhea or severe headaches.
Type I allergy can be detected relatively easily by a general practitioner or an internist. Further treatment depends on the cause and also on the severity of the symptoms, so that no general prediction is possible.
Treatment & Therapy
There are various therapeutic measures against Type I allergies: So-called antihistamines can be taken purely symptomatically, which prevent the release of the messenger substances involved. This works better for some patients and worse for others.
Emergency sprays, which actively dilate the bronchi after inhalation, help against asthma attacks. This works very well for most asthmatics. In worse emergencies, an emergency doctor always has so-called glucocorticoids in his luggage, e.g. Cortisol, which is injected into the vein and can slow down the body's defensive reactions.
In addition to these purely symptomatic measures, there is also the long-term option of desensitization therapy. By slowly increasing doses of the triggering antigen over a period of months, an attempt can be made to get the body used to the substance and at the same time to get rid of the allergic reaction. With some allergies such as Hay fever often works well for others, such as Animal hair only rarely.
prevention
When it comes to prevention, there are various theories: What is certain is that everyone has a different tendency to allergic type I reactions. If both parents are asthmatic, the risk of having an asthma attack is significantly higher than in the "normal population". 10% of all people in Germany have them Type I allergies, in so far the word "normal population" is put in quotation marks.The proportion is even higher for children.
At the same time you can do something good for your children if you let them come into contact with dirt: The so-called "hygiene hypothesis" states that children who grew up on farms and played a lot outside are significantly less likely to get allergies than children from Downtown households. Too much hygiene increases the risk of a type I allergy.
Aftercare
The first treatment usually only combats the symptoms of a type I allergy. In many cases, however, targeted follow-up care in the form of desensitization or specific immunotherapy (SIT) can be useful. In this way, the allergy is treated over the long term.
As part of the desensitization process, the allergy sufferer's immune system should gradually become accustomed to the substances that are responsible for the occurrence of type I allergies. So far, desensitization has been the only way to counter the causes of an allergy. The specific immunotherapy makes it possible to improve the symptoms and prevent secondary diseases.
Often the allergy sufferers can even be relieved of the symptoms of the allergy in the long term. As a rule, however, it only works if you have a type I allergy. So it must be an allergy of the immediate type. During follow-up care, the allergen that is causing the allergic reactions is administered at regular intervals to the allergy sufferer. The dose increases as the treatment progresses.
Specific immunotherapy is divided into an initial phase and maintenance therapy. During the initial phase, the patient is given a syringe with an allergen extract under the skin every week. If the dose is finally tolerated, maintenance therapy begins, during which the highest possible dose is injected once a month. As a rule, classic immunotherapy takes up to three years.


.jpg)




.jpg)


.jpg)


.jpg)




.jpg)