The germ Ureaplasma urealyticum belongs to the family of Mycoplasmataceae and the genus of ureaplasma.
What is Ureaplasma urealyticum?
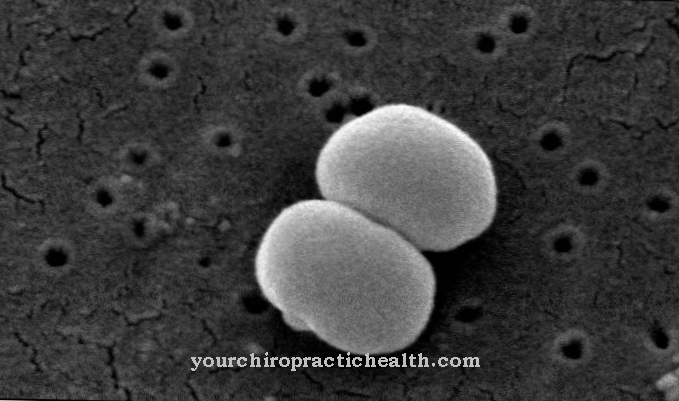
Ureaplasma urealyticum is a germ of the class of the Mollicutes. Like other germs of this class, it is characterized by a missing cell wall and a pleomorphic shape. Due to the missing cell wall, the pathogen is gram-negative. Further properties such as natural penicillin resistance and the possibility of shape change (pleomorphic shape) are made possible by the missing cell wall.
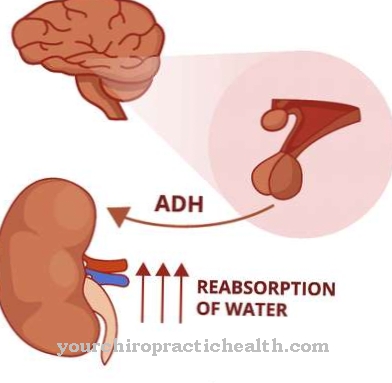
In contrast to mycoplasma, ureaplasma is able to split (lysis) and break down urea. Like other germs of the Mycoplasmataceae family, they parasitize both intra- and extracellularly. A settlement in the urogenital system and especially in the urethra is advisable due to the characteristic ability to break down urea.
The properties of the pathogen can be derived from the origin of the name: The class designation "Mollicutes" means "soft-skinned" (Molli = plump, soft) and indicates the missing cell walls. The family name "Mycoplasmataceae" roughly means "mushroom-like" (Mycos = mushroom) and alludes to the pleomorphic form of the germs, which is at times elongated and looks like a mushroom. The species name Ureaplasma urealyticum indicates the pathogen's ability to break down urea, i.e. urea.
Mollicutes class germs were isolated for the first time in cattle with pulmonary disease (pleuropneumonia) in 1898. The assumption that it was a primordial germ, which was also reinforced by the very small genome (580kbp), could only be refuted by precise DNA sequencing.
Germs of the Mollicutes class are products of degenerative evolution. Mollicutes are degenerate forms of a Lactobacillus species. The species Ureaplasma urealyticum represents a further development of the original Mollicutes and is the most important representative of the genus Ureaplasma in human medicine. A close examination of the genome revealed that Mollicutes rejected a significant part of their original DNA. With 580–2,300 kbp, they are among the organisms with the smallest genome available. For comparison, the genome of the E. Coli bacterium has a size of 4,500 kbp and the genome of Homo Sapiens has a size of 3,400,000 kbp.
Due to the small size of 200 nanometers, germs of the Mollicutes class are considered laboratory contaminants. The serial production of sterile filters only allows a pore density of 220 nanometers, which does not guarantee effective filtering of germs of the Mollicutes class.
Occurrence, Distribution & Properties
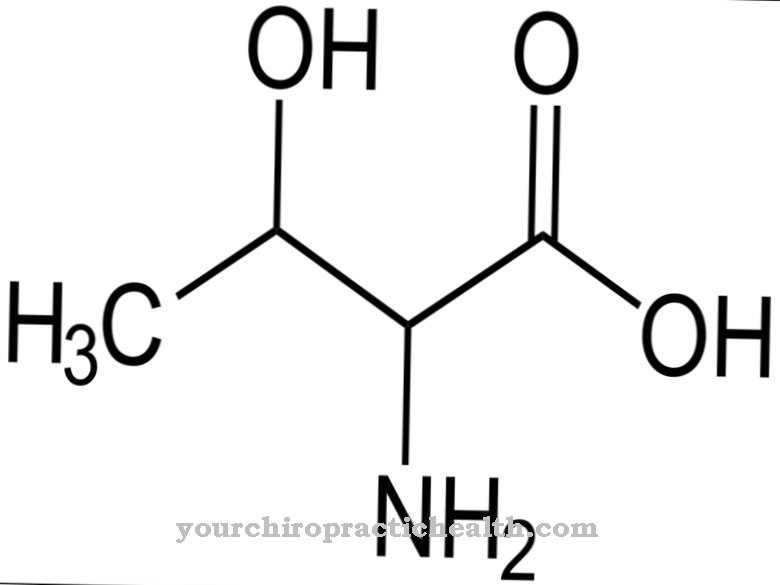
Germs of the Mycoplasmataceae family have rejected considerable parts of the original DNA and are therefore dependent on essential metabolic components from other cells. Due to the rejected parts of the genome, mycoplasmas are not able to produce or break down amino acids, nucleic acids and fatty acids themselves and have to pull them from other cells.
The ability of ureaplasma to break down urea is ideal for parasitic colonization of the urogenital system.
Illnesses & ailments
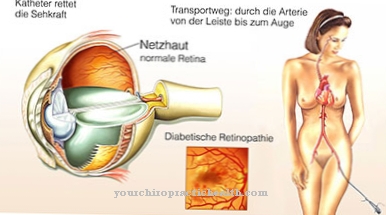
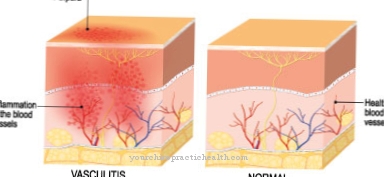
The bacterial species Ureaplasma urealyticum is considered to be facultative pathogenic and can colonize the mucous membranes of the lower female genital tract without complications. In the male genitourinary system, aggressive and rampant infections are more common. Starting in the urethra, cystitis develops, which can spread to the testicles, prostate and kidneys. The inflammation causes severe pain and fever and, if left untreated, can lead to sterility.
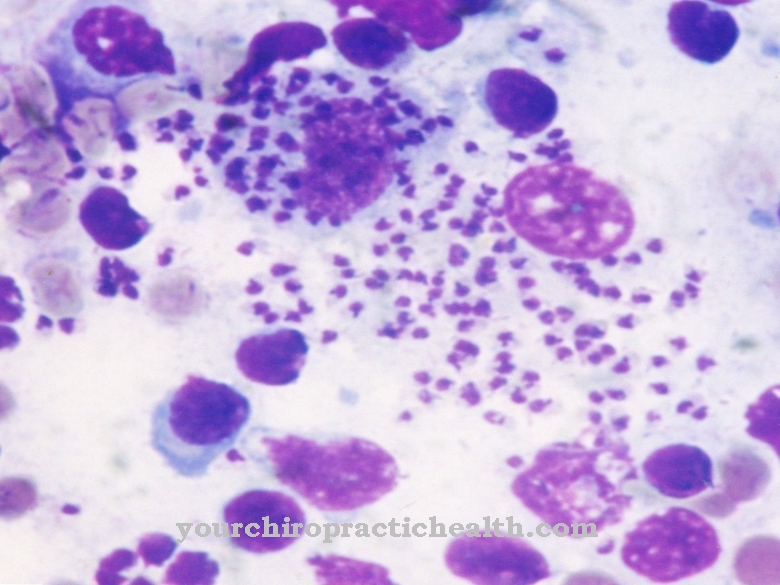
The germ settles unnoticed in the vaginal mucous membrane and can be found regularly during gynecological examinations. Infection of the child can occur during pregnancy and especially during childbirth. In infants, the germ can cause severe pneumonia and chronic infections of the central nervous system. In particularly severe cases, the germ triggers newborn sepsis which, if left untreated, can lead to the death of the infant.
Newborn sepsis causes around 5% of all child deaths under the age of 5 worldwide. Newborn sepsis is favored by an immune deficiency and malnutrition in the infant and is therefore a disease that occurs particularly in poorer countries. Newborn sepsis is not only triggered by ureaplasma, but can also be caused by streptococci, staphylococci and many other germs.
Due to the large selection of potential pathogens, spontaneous antibiotic treatment is not advisable. Since Ureaplasma has a natural resistance to penicillin and other antibiotics that attach to the cell wall due to the lack of cell walls, and since many other pathogens are now equipped with a large number of antibiotic resistances, a precise clarification with the aid of laboratory medical findings seems essential. The exact nature of the pathogen including a resistance determination is also important in order to avoid a persistent manifestation of the pathogen.
Since persistent forms of pathogens from the families of the Chlamydiaceae and Mycoplasmataceae have been observed through the administration of penicillin, extreme caution is required here.A hasty and instinctive decision in favor of conventional antibiotic treatment can lead to serious complications and can lead to the development of further resistances. A spontaneous antibiotic therapy without clarification of the exact causes can therefore be assessed as gross negligence.
To combat inflammation caused by Ureaplasma urealyticum, macrolide and tetracycline antibiotics are recommended. These groups of antibiotics work inside the cell and inhibit the pathogen's protein synthesis. Auto-replication can thereby be inhibited and a competent immune defense is promoted.





.jpg)









.jpg)


.jpg)
