The Urothelial carcinomawhich occurs predominantly between the ages of 60 and 70, is often the result of nicotine consumption and / or bypassed urinary tract infections and bladder infections. In the early stages, various treatment methods are possible, while in later stages the success in healing is poor.
What is urothelial carcinoma?
As Urothelial carcinoma the medical practitioner describes malignant (malignant) tumors that are located in the area of the tissue of the lower urinary tract. Occasionally, the tumors can also occur as cancer of the ureters, the renal pelvis, the urethra or in the form of bladder cancer.
The majority of those affected become ill between the ages of 60 and 70. About five percent of all urothelial carcinomas are located in the ureters or in the renal pelvis; in the remaining cases, however, the urothelial carcinoma forms in the urinary bladder.
causes
One of the most common causes is smoking. In particular, chronic irritation of the mucous membrane cells in the bladder, which subsequently leads to bladder infections that have not healed completely and which causes bladder stones, can also promote urothelial carcinoma.
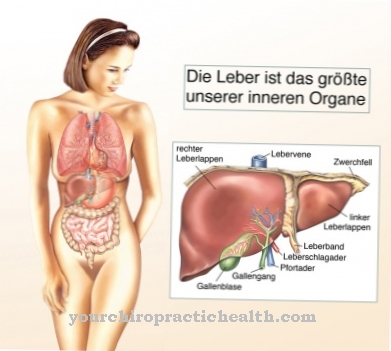
Schistosomiasis (worm infestation of the bladder, intestines, liver or genital organs) can sometimes increase the risk of urothelial carcinoma. Other favorable factors are hair dyes and chemical substances that have been shown to have carcinogenic substances.
Symptoms, ailments & signs
The first sign of urothelial cancer is a clearly visible admixture of blood when urinating (so-called hematuria). Furthermore, the person concerned complains of problems or disturbances when urinating. Emptying the bladder is painful; pain often occurs in the bladder area for no reason.
If the tumor is at the point of entry of the ureters, the carcinoma can obstruct the flow of urine in such a way that urinary retention occurs. In that case, patients complain of flank pain. Urothelial carcinoma causes symptoms similar to those of a bladder infection. For this reason, it is important that people who have these symptoms and are over 40 years of age consult a doctor so that urothelial carcinoma can be ruled out.
Diagnosis & course of disease
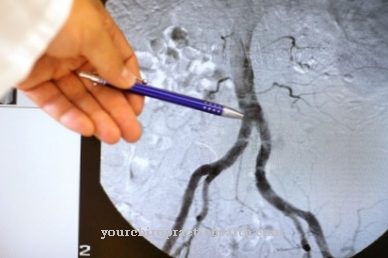
The doctor not only checks the patient's medical history, but also tries to find any cancerous tumors in the bladder by performing a thorough abdominal examination and observing the symptoms. To do this, he uses ultrasound, with which tissue changes can be detected. Doctors can use blood and urine tests to rule out cystitis.
It is important that the inside of the urinary bladder is examined using an endoscopic procedure. As part of the examination, tissue samples (biopsy) are also taken, which are then intended to provide information about whether a urothelial carcinoma is actually present. If the suspected diagnosis is correct, further examinations will be carried out. The doctor then has to determine the extent of the urothelial carcinoma. Using magnetic resonance imaging or computed tomography, it is possible to determine the stage of development of the tumor.
The doctor then divides the urothelial carcinoma into a TNM classification, whereby the size of the tumor, any metastases and lymph node involvement are checked and documented. If the tumor has already affected the deep tissue, the prognosis is negative. In around 70 percent of all cases, however, urothelial carcinoma is discovered at an early stage, so that a full recovery is possible; if the entire tumor is removed, the patient has the opportunity to survive the disease.
Complications
Since urothelial carcinoma is a cancer, in the worst case it can lead to the death of the person affected. The other complications and complaints therefore also depend very much on the exact form of the tumor. For this reason, a general forecast is usually not possible.
Sometimes those affected suffer from bloody urine. This symptom can also lead to a panic attack in some people. Urination is also associated with pain. The bladder itself can hurt for no particular reason. The pain often spreads to the flanks, so that the patient's quality of life is significantly restricted by the urothelial carcinoma.
If metastases have already formed, treatment of the urothelial carcinoma is usually no longer possible and the person concerned dies prematurely. In some cases, however, the tumor can be removed by surgery. There are no complications, but those affected continue to suffer from kidney failure and need a donor kidney or dialysis. Urothelial carcinoma significantly reduces the patient's life expectancy.
When should you go to the doctor?
Urothelial cancer must always be treated by a doctor. It is a serious illness, which in the worst case can also lead to the death of the person concerned. Therefore, a doctor should be consulted at the first symptoms and signs of the disease. In the case of urothelial cancer, a doctor should be consulted if the person concerned has bloody urine. This complaint can also occur sporadically.
Furthermore, urination itself is associated with severe pain, so that in some cases those affected also suffer from mental disorders or from depression. Furthermore, pain in the flanks or in the lower area of the abdomen can indicate urothelial carcinoma. Patients over 40 years of age in particular should consult a doctor with these symptoms so that the urothelial carcinoma can be detected and removed at an early stage. Further treatment depends on the extent of the tumor. The disease may also lead to a reduced life expectancy for the person affected.
Therapy & Treatment
The treatment depends mainly on the extent of the tumor. If the tumor has already reached the bladder wall or has nested itself in the surrounding tissue, the doctor speaks of an advanced stage. However, it is possible that tumors that have only spread to the mucous membrane of the bladder can be removed endoscopically - via the patient's urethra.
That treatment is called Transurethral Electroresection (TUR). However, this method is only used for superficial tumors. It is important that the urinary bladder is flushed afterwards. A regression of the tumor can be prevented by means of immune or chemotherapeutic agents. Tumors that have already grown directly into the muscle of the urinary bladder must be removed along with the bladder.
The patient then receives an artificial urinary bladder, which consists of the small intestine and the urethra. With this variant it is possible that the patient can be cured. However, if it is not possible to remove the bladder or to form an appropriate replacement because it is a patient in need of care or a person with kidney failure or also a patient who already has a tumor in the urethra, the urine is passed through the abdominal wall ( via a short piece of intestine) is secreted directly into a bag.
In a few cases, partial removal of the urinary bladder can also be successful. There are also so-called combined chemo-radiotherapies. However, this therapy is only carried out in selected patients. If it is a metastatic urothelial carcinoma, the doctor can use chemotherapy to destroy the rapidly growing cancer cells.
Radiation - that is, radiotherapy - is usually only carried out before a surgical procedure; Sometimes radiotherapy can also be used as part of follow-up treatment.
prevention
It is important that all risk factors - such as smoking - are given up if urothelial carcinoma is to be prevented. Above all, people who deal with carcinogenic substances should rely on their protective measures and take regular preventive examinations. It is important that urinary stones and any urinary tract infections are treated consistently so that there is no chronic course of the disease that not only provokes the mucous membrane cells, but sometimes also promotes the formation of urothelial carcinoma.
Aftercare
After the actual treatment of the urothelial carcinoma, follow-up care is initiated. The focus is on the timely detection of a possible relapse. For this reason, check-ups are carried out at short intervals. They include regular ultrasounds and urine tests.
In the case of bladder-preserving therapy, a cystoscopy (bladder mirror) is also used. If a radical cystectomy has been performed, imaging tests such as computed tomography (CT) or magnetic resonance imaging (MRI) follow. If there are no abnormal findings over a longer period of time, the intervals between the individual examinations can be extended.
After a cystectomy and urinary diversion, follow-up treatment is required that adapts to the special needs of the patient. However, it is only considered useful when accompanying chemotherapy has ended. In the context of rehabilitation, the focus is on postoperative functional disorders.
These primarily include bladder emptying disorders, urinary incontinence, dealing with a urostoma and impaired sexual function. In the case of older patients, the therapists adapt the treatment to their physical and mental capabilities. Working patients should be able to return to work.
If lymphedema appears on the legs after treatment for urothelial carcinoma, the affected person is given special compression stockings or elastic wraps. Manual lymph drainage is also helpful if lymphocele can be ruled out. As part of aftercare, the patient's quality of life is usually the focus. Among other things, questionnaires about quality of life can be filled out.
You can do that yourself
Urothelial carcinoma is associated with various symptoms. Patients can relieve these symptoms on their own by following a healthy lifestyle and taking some supportive measures.
First of all, it is advisable to change your diet, because carcinomas lead to gastrointestinal complaints such as stomach irritation or heartburn. An adapted diet reduces the symptoms by relieving the stomach and increasing wellbeing. In addition, a diet rich in vitamins and minerals supplies the body with all the substances it needs to fight urothelial carcinoma. For pain in the bladder or urinary tract, simple home remedies such as cooling or hot compresses, massages and treatments with pain relieving oils and ointments can help. Sufficient sleep inhibits the sensation of pain. Those affected pay attention to a well-ventilated bedroom so that the night sleep is restful.
At the same time, distraction helps to forget the pain. Patients can pursue their hobbies or spend time with other people. Conversations with other affected people are felt to be particularly liberating. Suitable contact points are, for example, self-help groups or internet forums. Sick people can find like-minded people there who can give valuable tips on how to effectively support urothelial cancer therapy.



.jpg)

.jpg)






.jpg)




.jpg)

