Visceral leishmaniasis (Kala Azar) is an infectious disease that can be traced back to a parasitic pathogen (Leishmania) that is widespread in tropical and subtropical areas. Depending on the pathogen subtype, visceral leishmaniasis can be severe.
What is visceral leishmaniasis?
As visceral leishmaniasis (kala azar) is an infectious disease that is rarely found in Germany and is due to the transmission of the parasitic infectious agent (Leishmania) by insects (butterfly mosquitoes, sand flies).
The pathogens of visceral leishmaniasis belong to the class of protozoa (animal unicellulars), the so-called mastigophora (also: flagellates), which are widespread in Asia (especially India), Africa, South America and the Mediterranean region. In most cases, those affected become infected with the pathogen while traveling to these countries.
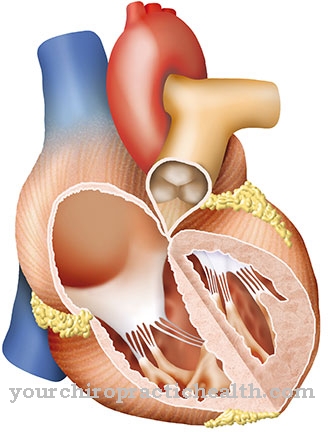
While other forms of leishmaniasis affect the skin (cutaneous leishmaniasis) or the skin and mucous membrane (mucocutaneous leishmaniasis), the most severe forms of leishmania, visceral leishmaniasis, affect the internal organs, particularly the spleen, liver, lymph nodes, and bone marrow. In addition, skin changes in the form of dark spots can occur, from which the Indian expression for visceral leishmaniasis Kala Azar ("black skin") is derived.
causes
The visceral leishmaniasis is caused by a parasitic pathogen (Leishmania donovani, L. chagasi, L. infantum) belonging to the class of Mastigophora. Infection with visceral leishmaniasis occurs via stings from certain types of insect (sand flies) that have previously become infected in infected vertebrates (mouse, wolf, dog).
After the insect bite, the leishmanias invade the monocyte-macrophage system which, in cooperation with the lymphocytes, participates in immune regulation and eliminates degradation and foreign substances, and reproduces.
The monocyte-macrophage system includes the reticular connective tissue in lymphatic organs, the Kupffer stellate cells of the liver and histiocytes of the skin. These organ systems are accordingly severely affected. In addition to indirect infection through insect bites, direct transmission through organ transplants and blood donations is possible.
Symptoms, ailments & signs
The symptoms of visceral leishmaniasis (kala azar) depend on the type of pathogen and how strong the patient's immune system is. There are infections that are symptom free, but the disease usually affects the bone marrow, liver, spleen, or lymph nodes. The disease can either begin insidiously or break out suddenly, with the patient then suffering from a very strong feeling of illness.
Typical symptoms include lymph node swelling, weight loss, diarrhea or abdominal pain. Often the spleen and liver are also swollen, which can then be recognized by a distended stomach. Changes in the blood count also occur. For example, those affected suffer from blood clotting disorders or anemia.
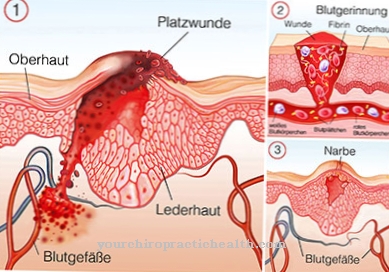
Skin changes often occur, with dark red papules or brown-black spots appearing. As the disease progresses, the skin turns gray. For this reason, visceral leishmaniasis is also called kala azar ("black skin"). After one to three years, those affected can develop what is known as post-kala-azar skin leishmaniasis. Reddish or light-colored spots appear on the body or face, which then become lumps or papules and whose appearance is also reminiscent of the leprosy disease.
Diagnosis & course
The visceral leishmaniasis manifests itself after an incubation period of 10 days to 10 months (sometimes longer) on the basis of characteristic symptoms such as creeping or sudden onset of the disease with remitting fever lasting for weeks, abdominal pain, hepatosplenomegaly (enlarged liver and spleen), swelling of the lymph nodes, pronounced hypochromic anemia (hemoglobin deficiency) (Platelet deficiency) as well as dark, blotchy skin pigmentation, amyloidosis (protein deposits) and cachexia (emaciation).
Visceral leishmaniasis is confirmed on the basis of a pathogen detection in bone, spleen, liver or lymph node aspiration. In the advanced stage of the disease, in some cases of visceral leishmaniasis a puncture is no longer possible, so that the diagnosis is confirmed by means of serological examinations (immunofluorescence method, ELISA technique). A Leishmanin reaction test can be performed to determine the immune status of the person affected.
The course of visceral leishmaniasis depends to a large extent on the pathogen subtype. While Leishmania chagasi and Leishmania infantum often cause no symptoms and heal by themselves, the in many cases protracted infections with Leishmania donovani can be fatal if untreated.
Complications
At Kala Azar, those affected suffer from various skin changes. These have a very negative effect on the aesthetics of the person concerned and can also lead to inferiority complexes or to a significantly reduced self-esteem in the patient. In children, the disease can also trigger bullying or teasing.
Furthermore, kala azar leads to the formation of ulcers and furthermore to severe weight loss in the patient. Those affected sometimes suffer from diarrhea and vomiting and can also feel severe pain in the abdomen. Furthermore, the affected person's lymph nodes swell and a fever occurs.
The patients appear exhausted and tired and can therefore no longer perform strenuous activities. As a rule, the disease has a negative effect on the life and everyday life of the person affected. In most cases, kala azar can be treated relatively well with the help of medication.
There are no particular complications and the symptoms are significantly alleviated. In some cases, however, the drugs can cause side effects. Successful treatment will not reduce the patient's life expectancy.
When should you go to the doctor?
A doctor should be consulted if health disorders arise during a stay in African, South American or the area around the Mediterranean. If the changes in health occur after a visit to the region there, the person affected also needs a clarification of the complaints. Basically, however, it is important to find out about the local health conditions immediately before starting a trip.
It must be clarified which diseases are to be expected and how transmission can take place. If necessary, vaccinations are recommended. If swelling of the lymph glands, changes in the complexion or unwanted weight loss are noticed after an insect bite, action must be taken. If you have diarrhea, stomach pain, nausea and a general feeling of illness, it is advisable to consult a doctor. The cause must be clarified and a diagnosis is necessary.
This is the only way to develop a treatment plan that can help alleviate the symptoms as quickly as possible. In order to avoid complications and minimize risks, it is necessary to consult a doctor if you feel unwell, develop lumps on the skin or discolouration is observed. Internal weakness, circulatory disorders and an increased need for sleep are further signs of an existing illness. Since organic changes in visceral leishmaniasis can occur, immediate action should be taken at the first signs.
Treatment & Therapy
The visceral leishmaniasis is treated systemically with Ambisome (liposomal amphotericin B). Liposomal amphotericin B is in most cases well tolerated and is infused intravenously as part of a 10 to 20 day therapy.
In the case of intolerance or non-response to therapy with liposomal amphotericin, miltefosine and pentavalent antimony preparations are used alternatively in visceral leishmaniasis. Miltefosine is given orally in tablet form twice a day for one month and causes only minor gastrointestinal discomfort (episodic diarrhea or vomiting).
Pentavalent antimony (sodium stibogluconate, meglumine antimonate), on the other hand, are injected intramuscularly or intravenously by the doctor as part of an average of 28 days of therapy in the hospital, with prolonged dull pain at the injection site as well as nausea and headache being side effects.
In some cases, therapy with antimony is ineffective in visceral leishmaniasis because the infectious agents have developed resistance to this active ingredient. Pentamidine and the antibiotic paromycin are also used as antiprotozoal agents against visceral leishmaniasis.
Pentamidine, however, leads to pronounced side effects and, among other things, affects glucose metabolism disorders (diabetes mellitus) in over 10 percent of those affected.
prevention
There one visceral leishmaniasis is transmitted to humans via insects, appropriate precautionary measures should be taken to protect against mosquito bites when traveling to areas such as Asia, primarily India, Africa, the Mediterranean region and South America. This includes wearing suitable, long-sleeved clothing and using a close-meshed mosquito net while sleeping. So far there is no vaccination against visceral leishmaniasis.
Aftercare
Since visceral leishmaniasis affects the internal organs, an intensive follow-up treatment should always take place on successful therapy. The early detection and timely treatment of secondary diseases of the organs is central here. Accordingly, even after successfully treated visceral leishmaniasis, regular measurements of the organ values in the blood should be carried out.
In particular, the organs that were affected by visceral leishmaniasis should also be regularly examined with imaging methods (MRT, CT, X-ray, ultrasound) so that hidden organ damage that is not yet visible in the blood can also be detected. If the skin was also affected by visceral leishmaniasis, the relevant areas must be regularly examined by a dermatologist, whereby tissue samples should be examined for the pathogen to be on the safe side.
In addition, people formerly suffering from visceral leishmaniasis should avoid traveling to areas (Asia) where the disease-carrying sand fly lives. If such trips cannot be avoided, intensive mosquito repellants and skin hygiene should be observed in order to avoid a recurrence of visceral leishmaniasis. Mosquito nets should be very close-meshed (1.2 millimeters) as the sand mosquito is very small. In addition, you should spray yourself several times a day with mosquito repellent sprays such as Autan (so-called repellents). In addition, you should shower daily. The face, neck and hands should also be covered with fabric if possible.
You can do that yourself
The drug therapy of visceral leishmaniasis can be supported by the patient's own initiative. First of all, it is important to pay attention to typical side effects such as kidney pain or hypersensitivity disorders. If pain or other complaints occur, the doctor must be informed. After intravenous treatment, bed rest is recommended in order to quickly cure side effects such as headache and body aches.
The cause of visceral leishmaniasis needs to be determined in order to avoid re-infection. Kala-azar is mostly transmitted by insects. Therefore, a suitable insect repellent must be used on future trips. Affected people should wear suitable clothing and sleep with a fly net at night. People who have already had kala-azar are no longer allowed to participate in the blood donation. This safety precaution serves to prevent the pathogen from being transmitted to other people. The blood donation ban must be strictly adhered to, otherwise severe penalties are imminent.
Finally, attention should be paid to unusual symptoms after illness. In individual cases, the pathogen returns after months or even years and causes serious health problems. A comprehensive prophylaxis in the form of regular check-ups is therefore absolutely necessary.








.jpg)



.jpg)










.jpg)
