The term Wound healing disorders denotes general difficulties in natural wound healing. This can occur for a wide variety of reasons, for example previous illnesses or incorrect wound care.
What are wound healing disorders?
From Wound healing disorders Doctors always speak when there are difficulties or delays in natural wound healing. Basically, the body tries to replace the tissue injured by violence or illness with healthy tissue as quickly as possible.
Due to various causes, however, the healing process can be disrupted. This is a burden for the organism, especially since there is a constant risk of inflammation of the open wound. Particularly in the case of very large and serious wounds, for example after an operation, life-threatening conditions can result. Surgical interventions must therefore be carefully considered in the case of certain diseases.
causes
The causes for Wound healing disorders can be diverse. In general, wounds heal better in young people than in older people. Inadequate wound care is often responsible for the impaired healing process.
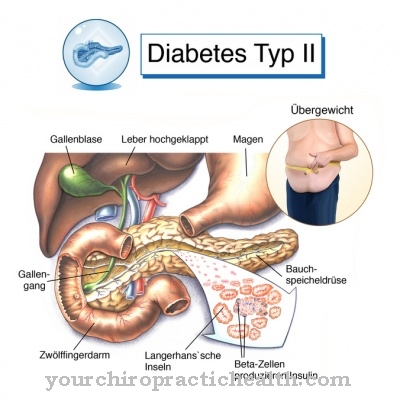
If the wound was not closed perfectly after an operation or the sutures are removed too early, it cannot close optimally. The individual health of the patient can also impair wound healing. Diseases such as diabetes, tuberculosis, HIV or drug addiction can cause wound healing disorders, as can certain drugs.
A lack of protein, a lack of vitamins or being very overweight are other factors that can lead to problems with wound healing. The attending physician should therefore always take the patient's lifestyle into account when making a diagnosis.
Symptoms, ailments & signs
Wound healing disorders can have serious consequences. It is therefore important to watch out for the first signs of impaired wound healing. This enables prompt, professional treatment by a doctor. Some clinics have special specialists who take care of wound care for amputation-related and other wound healing disorders.
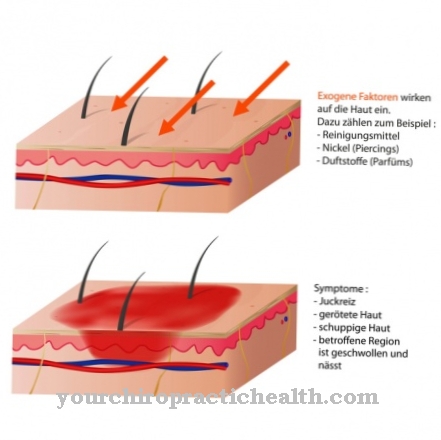
The most important symptom of wound healing disorders is that an open wound simply does not want to heal. This could be an open leg, an amputation or surgical scar, or some other type of wound. The wound defect can show up at different times. The wound may ooze or bleed without showing sufficient signs of healing. The area around the wound may be very painful, swollen, or discolored.
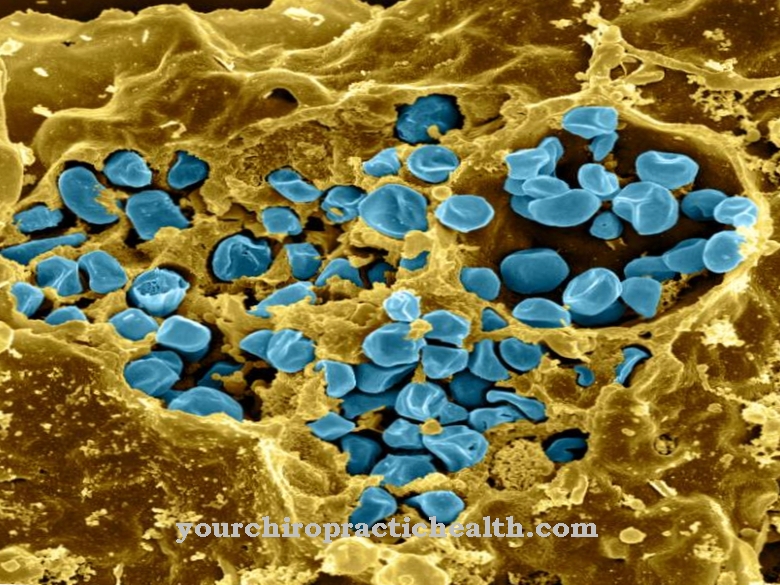
In addition to the wound healing disorders, nerve, bone and vascular damage sometimes occur. If the blood and lymph circulation in the wound area is disturbed, lymphedema and other sequelae can occur. Wound infections can develop. Their symptoms are a foul odor, a purulent layer on the wound and redness in the wound area. There is pressure pain around the open wound. A fever can indicate the onset of blood poisoning.
The main symptoms of wound healing disorders are delayed healing, reddening, overheating, tenderness or swelling. The wound may ooze, bleed, or fester. There is pain in the wound area and sometimes restricted mobility.
Diagnosis & course
Mostly can Wound healing disorders can be optically diagnosed directly by the attending physician. By looking at and examining the wound, he can determine how old it is and to what extent it should have healed within the framework of optimal wound healing.
If there is actually a wound healing disorder, the exact causes must be determined. For this purpose, both wound care and the patient's living conditions should be considered more closely. If a wound remains untreated while the healing process is disturbed, severe inflammation can result.
In the worst case, it can threaten the patient's life, especially if the wound is large. Appropriate medical care is therefore essential.
Complications
Wound healing disorders are considered a dangerous complication in operations, injuries, and underlying diseases. They occur particularly in people with a weakened immune system or as a result of diabetes mellitus and serious skin diseases. However, an incorrect position after the operation or an incorrect treatment of the wound can lead to impaired healing.
With optimal wound treatment, the chances of recovery are good. However, relapses can occur again and again. The prognosis of a wound healing disorder also worsens if it is caused by an underlying disease. Then complete healing of the wound is only possible if the causative disease is treated successfully.
Wound healing disorders can lead to serious complications. If the wound is not disinfected or only insufficiently disinfected, there is often a rapid increase in pathogens that penetrate the wound. Foci of pus develop, which in very unfavorable cases can lead to potentially fatal sepsis. Furthermore, wound healing disorders are often the cause of chronic nerve, vascular, muscle, tendon or bone damage.
A particularly feared complication of wound healing disorders is the so-called compartment syndrome. The tissue pressure in the muscles increases as a result of the outflow disorders of the venous blood. The following blood circulation disturbance can interrupt the arterial blood flow to the muscles. Muscle tissue then often dies, especially in the lower legs, feet or forearms.
When should you go to the doctor?
Under optimal conditions, the symptoms of a wound decrease in a continuous process over several days or weeks. A doctor is not required if an improvement in health can be perceived daily. Frequently, there are states of tension during movement sequences, since the skin of the wound has not yet fully regenerated and is consequently not sufficiently flexible. This is a natural process that does not require any further medical care. A doctor is needed if the wound healing process has stopped progressing for several days. In addition, a doctor should be consulted if the symptoms increase.
Swelling and discoloration of the skin should normally decrease steadily. However, if they gain weight or if pain occurs, action is required. If the skin around the wound is irritated, action is also required. In particularly severe cases and if the healing process is unfavorable, blood poisoning can occur. Therefore, a hospital must be visited or an ambulance alerted if severe pain occurs, an intense malaise develops or edema develops. Sensitivity to pressure in the area of the wound is normal. Nevertheless, a doctor should be consulted if the tenderness becomes more intense or the affected area enlarges.
Treatment & Therapy
After a thorough examination and diagnosis by the attending physician, cleaning the wound is the top priority. It must be thoroughly cleaned and disinfected to prevent dangerous inflammation. Various rinsing solutions are available for this purpose.
Under certain circumstances, it may be necessary to surgically remove the already dead tissue and then sew the wound (again) so that healing can take place. Nowadays, wounds are generally covered with compresses over a large area so that natural healing cannot be impaired by external influences. These associations must be changed regularly.
In some circumstances, anticoagulant medication can also be administered. In addition to the acute care, it should also be found out what causes the Wound healing disorder ideally before the initiation of therapy. For certain diseases, special treatments are necessary or some medications may not be used. If the reasons for impaired wound healing lie in the patient's lifestyle, the nutrients or vitamins given can usually provide a remedy very quickly.
If diabetes is already present, the blood sugar level should always be regulated to an acceptable level. If the wound has already become infected, it must be treated quickly with medication or possibly also surgically so that life-threatening conditions cannot arise.
prevention
Wound healing disorders can in many cases be prevented through optimal and professional wound care. Great importance should therefore always be attached to this. Risk factors such as obesity or a lifestyle that promotes deficiency symptoms should be minimized so that in the event of a wound there are no major problems with the healing process. If there are underlying diseases such as diabetes, appropriate treatment is urgently needed. If a wound does not heal quickly and easily as usual, a visit to a doctor is strongly recommended.
Aftercare
There are various complications in wound healing disorders. However, follow-up care should not be related to the original wound alone. First of all, it must be ensured that the wound does not become infected or that inflammation is recognized and treated as quickly as possible. In addition to local measures, it may also be necessary to take certain medications, such as antibiotics.
It is therefore important to have a doctor regularly monitor wound healing. The second pillar of follow-up care is to determine the cause of a wound healing disorder. In some cases, previously unrecognized systemic diseases (for example diabetes) are responsible for this, but also extensive cigarette consumption. It is important to treat the actual cause, as otherwise the recurrence of wounds can lead to wound healing disorders that are increasingly difficult to treat - also depending on the type and location of the wound.
The patient should work with an experienced medical professional and seek advice and treatment for the individual case. The wound itself must be cared for until it has healed completely, if necessary bandaged and kept away from sources of infection. Repeated injuries can also lead to considerable complications, and it is advisable to take care of the affected body regions during aftercare up to a certain point in time.
You can do that yourself
In the event of wound healing disorders, increased care should be exercised in everyday movements. Feelings of tension should always be avoided in the area of the wound. Therefore, stretching or performing stretching exercises is not recommended. The physical strain must be adapted to the health possibilities. It is therefore necessary to check which sporting activities can be carried out and which professional activities can be carried out in the current health situation.
Situations of overexertion or heavy physical strain have a disruptive effect on the recovery process and must be avoided. The organism can be supported in healing through a healthy and balanced diet. A diet rich in vitamins, an adequate supply of oxygen and avoiding the consumption of harmful substances help. The immune system is supported and can promote the regeneration process more strongly. Sufficient sleep and regular rest have also proven helpful. Breaks should be taken at regular intervals and the wound should be checked several times a day.
The wound dressing must be changed in a sterile manner. If necessary, the help of nursing staff can be obtained. If possible, the physical region around the existing wound should be kept still. As a result, the fulfillment of day-to-day duties often requires the support of other people.

.jpg)


.jpg)











.jpg)