Under Xeroderma pigmentosum, also Moonlight sickness called, medical professionals understand a skin disease caused by a genetic defect. Those affected show pronounced UV intolerance and therefore usually have to avoid sunlight completely. The disease is so far incurable.
Xeroderma pigmentosum is a very rare, genetically determined disease of the skin and mucous membranes, which is mainly characterized by an over-sensitivity to ultraviolet light (UV light). Xeroderma pigmentosum has an unfavorable (unfavorable) course, which is usually characterized by skin cancer.
What is xeroderma pigmentosum?
Xeroderma pigmentosum is a serious skin disease that manifests itself through neurological failures and, above all, pronounced UV intolerance.
This leads to painful skin inflammation, which later develops into malignant ulcers. Since the disease often leads to an early death in the first decade of life, most of those affected are children, who are colloquially known as moonlight children.
However, there are also known cases in which those affected reached the age of 40. Xeroderma pigmentosum is very rare; however, there are strong regional differences. In Germany, around 50 children have the gene defect, in the United States there are around 250.
Moonlight sickness is therefore a genetic disease that manifests itself in childhood when the skin and mucous membranes are overly sensitive to UV light. Accordingly, typical symptoms of xeroderma pigmentosum are excessive sunburn reactions in the form of inflammation after very brief contact with sunlight (especially face, hands, arms), prematurely aging skin that is wrinkled and pigmented reddish-brown or freckle-like, and tumors on the skin and Eyes that can become malignant in the further course of the disease (squamous cell carcinoma, melanoma, basal cell carcinoma).
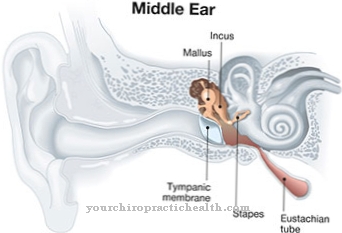
Xeroderma pigmentosum also causes telangiectasia (enlargement of the small blood vessels), keratitis (inflammation of the cornea) and neurological disorders (sensitivity disorders, movement disorders, hearing loss) in around a fifth of those affected. A total of seven or eight forms of xeroderma pigmentosum (A to G and V) can be differentiated depending on the specific manifestation of the genetic defect.
causes
The causes for Xeroderma pigmentosum lie in a genetic defect that is inherited recessively. The so-called repair enzymes of the DNA are damaged in this process and skin damage caused by UV radiation cannot be repaired as in healthy people.
Xeroderma pigmentosum can be traced back to an autosomal recessive genetic defect in the DNA repair system, through which the DNA damage caused by UV light can no longer be repaired by the skin and mucous membrane cells. The UV-B rays that are not filtered out by the earth's atmosphere cause the synthesis of thymidine dimers in skin cells, which are a combination of two thymidine building blocks.
In a healthy organism, these compounds, which are harmful to cells, are recognized by a DNA repair system made up of enzymes and released from the DNA. Since in xeroderma pigmentosum this repair system is disturbed by a genetic defect and a lack of the DNA repair enzymes or DNA involved in this process.
DNA endonucleases are present, these compounds are not dissolved, so that the affected skin or mucous membrane cells can die or degenerate into cancer cells. Accordingly, xeroderma pigmentosum is often accompanied by skin cancers in childhood.
Any exposure to the sun therefore leads to painful inflammation that cannot regenerate on its own. Doctors divide the disease into different types, depending on where exactly the defective gene is located.
Some of these types of diseases are not only characterized by the already mentioned hypersensitivity to sunlight, but are also associated with neurological disorders such as hearing loss, movement disorders or a significant reduction in intelligence. For a child to be born with xeroderma pigmentosum, both parents must be predisposed to it.
Symptoms, ailments & signs
Xeroderma pigmentosum manifests itself through such symptoms as extreme sensitivity to light, changes in pigmentation on the skin, eye diseases, neurological problems and the constant formation of new skin tumors. The sensitivity to light is noticeable even in small children.
After a short exposure to light, severe sunburn with difficult-to-heal blistering often occurs. This particularly affects the face, arms or legs. In some patients, however, the skin initially remains normal after exposure to the sun. However, a large number of so-called birthmarks later develop in all those affected, which are diagnosed as both benign and malignant skin tumors.
Basaliomas are the majority of malignant tumors, followed by spinaliomas and melanomas. As a rule, the basaliomas do not form metastases. However, they often lead to disfigurement of the face and the affected areas. Melanomas in particular grow very aggressively and are often the cause of early death in patients. Sometimes the first symptom of xeroderma pigmentosum is also the sensitivity of the eyes to light.
The patient initially reacts very shy of light. Chronic corneal and conjunctivitis later develop. The eyesight decreases. Later there is even a risk of complete loss of sight. Tumors can also develop in the eyes. This is where spinaliomas are most frequently observed. In the course of the disease, some of the patients also develop progressive neurological complaints, which can manifest themselves in the form of a reduced intelligence, paralysis and movement disorders.
Diagnosis & course
Xeroderma pigmentosum is usually diagnosed based on the symptoms that occur. If xeroderma pigmentosum is suspected, the treating doctor may do a DNA test to determine the exact type of the disease and then treat it appropriately.
Blood and / or skin analyzes can be used to make statements about how well the skin cells are able to repair DNA damage after contact with UV light. A genetic analysis can also determine which form of xeroderma pigmentosum is present in the person affected. Xeroderma pigmentosum has an unfavorable (unfavorable) prognosis, as malignant tumors usually appear in the advanced course of the disease and before the age of 20.
With early diagnosis and consistent application of protective measures against UV light, this can be positively influenced and over two thirds of those affected by xeroderma pigmentosum reach the age of 40.
The first signs of xeroderma pigmentosum are severe sunburn or inflammation that occurs very quickly. The skin discolors, dries out and ages quickly. Malignant tumors of the skin, but also of the eyes, develop from the inflammations that do not heal properly.
Because of this rapid formation of cancer cells, the life expectancy of those affected is rather low. The exact prognosis depends on the type of disease and whether it is recognized in time.
Complications
The disease Xeroderma pigmentosum can significantly limit the everyday life of the person affected and thereby also reduce the quality of life. Those affected primarily suffer from a very high sensitivity to sunlight, so that even brief exposure to the sun can cause burns and discoloration of the skin. Spots and redness develop on the skin, which can also be accompanied by itching.
The skin itself looks wrinkled from xeroderma pigmentosum and can be covered with scars. In many cases, the patients are ashamed of the symptoms, which can often lead to inferiority complexes and thus to a significantly reduced self-esteem in the patient. Especially in children, the symptoms can also lead to bullying or teasing, so that they suffer from psychological complaints.
The skin can also become inflamed. Those affected also very often suffer from sunburn as a result of the disease, which means that they are always dependent on sun protection or protective clothing. Since Xeroderma pigmentosum cannot be cured causally, only the individual symptoms can be treated. There are no particular complications, although there is no positive course of the disease. The disease may also reduce the patient's life expectancy.
When should you go to the doctor?
People who are exposed to intense sunlight often suffer from sunburn. A doctor does not always have to be consulted for this. In most cases, self-help measures are sufficient to achieve relief as quickly as possible. In addition, it must be checked whether changes and optimizations can be made in dealing with direct sunlight on the skin. As a preventive measure, sun protection creams can be applied and the time spent in direct UV light should be minimized. If, despite all efforts, burns or pain occur disproportionately quickly when the skin is exposed to the sun, a doctor's visit is necessary.
Sensitivity to light, impaired vision, or changes in the pigmentation of the skin are all signs of a disease. A doctor's visit is necessary so that the causes can be determined and a diagnosis can be made. Withdrawal from social life, behavioral problems or mood swings are indications of a health disorder.
Treatment & Therapy
Remains Xeroderma pigmentosum if left untreated, the life expectancy of those affected is only a few years. It is therefore essential to consult a doctor at the first suspicion and, if the diagnosis is made, to take appropriate steps.
There is no cure for xeroderma pigmentosum; Appropriate treatment can often significantly increase the life expectancy of those affected. This includes that sunlight must be consistently avoided. The sick are not allowed to leave the house at all during the day or only with UV-resistant special clothing. The windows must also be darkened accordingly and provided with UV-repellent film.
In the case of xeroderma pigmentosum, therapeutic measures have so far been limited to minimizing the symptoms and preventing skin cancer through consistent protective measures against UV light and regular check-ups by the dermatologist (dermatologist). This primarily includes avoiding daylight (moonlight children), wearing appropriate protective clothing, especially on the arms, neck and face, as well as UV glasses and sun creams with a very high sun protection factor.
In addition, it is recommended to have the windows of rooms in which those affected stay longer and longer during the day coated with a special UV light protection film. Promising results were achieved in clinical tests with a liposome lotion that was applied to the skin and supplied locally with DNA repair enzymes. In those affected by Xeroderma pigmentosum, a significant reduction in the proportion of thymidine dimers and thus the skin damage induced by it was found, although the sensitivity to UV light could not be completely normalized.
The tests for this therapeutic approach to Xeroderma pigmentosum were, however, stopped for the time being due to a lack of money. In addition, genetic engineering attempts are made to replace diseased skin areas with healthy skin cells (e.g. from the buttock area) that have been provided with functional DNA repair mechanisms or a normal copy of the defective gene. However, this treatment method for Xeroderma pigmentosum is still in an early research phase.
The necessity of these drastic measures usually results in severe social isolation, not least because of the lack of understanding by society. Regular visits to the doctor with extensive skin and eye examinations can prevent the development of malignant ulcers. Since the skin of those affected is generally very sensitive, it often needs creaming and special care.
If there is sunburn or inflammation, pain medication can be given temporarily. The exact type of treatment, however, always depends on the type of disease and the individual characteristics.
prevention
As it is with Xeroderma pigmentosum If it is a disease that is hereditary, prevention in the strict sense is not possible. If the genetic defect is present in potential parents, they should seek detailed advice from the gynecologist before becoming pregnant. If the disease is diagnosed in a child, appropriate medical steps should be taken as soon as possible so that the person affected can live as long as possible and as far as possible free of symptoms.
Aftercare
Xeroderma pigmentosum is an incurable disease. There is no treatment for the condition. Those affected should avoid any contact with UV rays or at least reduce it significantly. Solariums may not be used under any circumstances. Reducing the radiation there would only worsen the symptoms and, in general, the condition of those affected.
Sun exposure should also be avoided. The everyday life of those affected is considerably restricted by the sick. All activities as well as the profession must be adapted to the illness. Those affected are not allowed to go outside without appropriate sun protection. Especially in summer, those affected have to be extremely careful and not make rash decisions.
Those affected have to put on special UV protection, which prevents the rays from penetrating the organism. Clothing should also be adapted to the disease. The body should be completely covered. For example, hats protect the face from the penetration of UV rays.
The body should be covered with long pants and long tops. The illness represents a high burden for those affected. Sometimes it is advisable to undergo permanent psychological advice on how to deal with the illness. Those affected should also seek help and support from family members whenever possible.
You can do that yourself
With this disease, the person affected must reduce UV radiation to a minimum or avoid it completely. This has the consequence that the lifestyle is severely impaired. Natural and artificial UV light may therefore only be absorbed according to the possibilities and conditions of the organism. Offers such as solariums are to be avoided completely. The UV light there would lead to a rapid increase in problems. Direct sunlight should also be avoided.
In everyday life, the planning of leisure activities or professional activities must be adapted accordingly. The patient should never leave the house without appropriate sun protection. Especially in the summer months, no careless actions should be taken. The skin must be protected with creams that reduce or block the penetration of UV rays into the organism. In addition, clothing should be adjusted. It is advisable to cover the body almost completely with fabrics or protective accessories. Hats or umbrellas help to avoid exposure to UV radiation on the face. The other parts of the body can be well covered by wearing long pants or long tops. At the same time, it is important to ensure that the clothing is air-permeable and does not lead to a feeling of constriction.
Since the illness is a strong emotional burden, cognitive exercises should be used to support the mental powers.

.jpg)


.jpg)
.jpg)

















.jpg)



