A Duodenal ulcer (duodenal ulcer) is damage to the intestinal wall. In detail, there is a dripping and excessive gastric juice secretion that attacks the wall of the duodenum. In addition to smoking, stress and medication, the bacterium Helicobacter pylori can also be responsible for duodenal ulcer disease.
What is a duodenal ulcer?

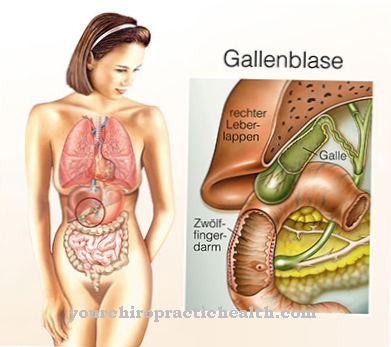
Of the Duodenum (duodenum) is an approximately 30 cm long, C-shaped part of the intestine and lies between the gastric outlet and the small intestine. The Duodenal ulcer (duodenal ulcer) is a deep substance defect in its wall. By definition, this defect extends deeper than the muscle layer below the mucous membrane.
An ulcer is the most common disease of the duodenum and is about five times as common as a stomach ulcer. If only the mucous membrane is affected, one speaks of erosion. Up to two percent of all people will develop a duodenal ulcer in the course of their life, men significantly more often than women. The frequency peak is in middle age.
causes
So a Duodenal ulcer can arise, there must generally have been a disproportion between protective and damaging factors. The most common cause is an infestation with a bacterium (Helicobacter pylori), which can be found in 90% of diagnosed duodenal ulcers. This can be done through certain adaptation processes, e.g. the formation of neutralizing enzymes that not only survive in the acidic environment of the upper gastrointestinal tract, but also multiply.
Additional damaging factors are the use of certain medications (e.g. diclofenac and aspirin), stress (physical and psychological) and circulatory disorders. A rare cause of a duodenal ulcer is a tumor disease in which the production of gastric acid is massively increased (by so-called gastrin-producing tumors). It has also been shown that people with blood group 0 are significantly more likely to develop duodenal ulcers; the cause is not yet fully understood.
Symptoms, ailments & signs
The symptoms of a duodenal ulcer are slow to develop. They only become more noticeable over the course of weeks and months. Typical signs at the beginning of the disease can be bloating and frequent flatulence. Heartburn and acid regurgitation can also appear as initial symptoms.
A small proportion of those with duodenal ulcer do not experience any symptoms in this first phase. The other sufferers feel an increasing dull pain in the upper abdomen. The pain can radiate into the back. Nausea and vomiting or loss of appetite can also be unspecific signs of a duodenal ulcer.
This can lead to an aversion to certain foods. Over time, unnatural weight loss can occur. A more classic symptom is when the pain occurs regularly on an empty stomach. This can be at night. Food intake usually leads to an improvement in the symptoms.
About every fifth duodenal ulcer is associated with bleeding, which is excreted in the stool or when vomiting and thus becomes visible. The stool shows a characteristic black color due to the mixture of blood and stomach acid (so-called tarry stool). Depending on the extent of the blood loss, circulatory problems can also occur. In individual cases the ulcer can cause life-threatening gastric perforation. This causes very severe pain in the pit of the stomach.
Course of disease
The symptoms of a Duodenal ulcer are completely unspecific at the beginning of the disease, so the diagnosis is often made late. Typical complaints are loss of appetite (with aversion to certain foods), nausea and pressure in the stomach area or a feeling of fullness in the middle upper abdomen. Unintended weight loss and stool abnormalities can also occur.
If the duodenal ulcer starts to bleed, it is not uncommon for black-colored stools to occur (so-called tarry stools). This is because blood turns black when it comes into contact with aggressive stomach acid (hematin formation). Tarry stools always require clarification and should therefore give cause for further investigation. In the case of sudden annihilation pain, a perforation (that is, a breakthrough of the duodenal ulcer into the free abdominal cavity) must be feared.
It is not uncommon for the sick to be completely asymptomatic and the diagnosis is made by chance. The diagnosis of a duodenal ulcer is made via a gastroscopy. As part of the investigation, a quick test for the typical Helicobacter pylori germ is always carried out. In addition, a small piece of tissue is sent in, which enables reliable detection or exclusion of an infestation with the harmful bacterium.
Complications
Bleeding is one of the most common complications of a duodenal ulcer. Older people are particularly at risk, and certain painkillers can also cause bleeding, especially large ulcers, if they are used for a long time. Minor bleeding often goes unnoticed, but can cause anemia: this is often discovered by chance during a routine examination.
Black stools, also known as tar stools, can indicate a bleeding ulcer. If larger vessels are affected, ulcer bleeding is often highly dramatic: Due to massive blood loss in a short time, there is a risk of life-threatening shock if the bleeding cannot be stopped by an immediate operation.
Another dreaded complication is the breakthrough of a duodenal ulcer into the abdominal cavity: The gastric contents escaping in the process can cause life-threatening peritonitis, so immediate emergency surgery is essential. Depending on the location of the ulcer, it can also penetrate the surrounding organs - such as the pancreas or the large intestine - and cause damage there.
If the ulcer is close to the exit of the stomach, it is not uncommon for a narrowing to occur, which hinders the further transport of the food pulp: Constant vomiting and massive weight loss can result. In very rare cases, a duodenal ulcer can become malignant and later form daughter tumors in other organs.
When should you go to the doctor?
If the person concerned suffers from uncomfortable gas, a feeling of pressure in the abdomen or pain in the lower abdomen, a doctor's visit is necessary. If there is a steady increase in health disorders within several days, weeks or months, a doctor is required. Swelling, a general malaise or a decrease in physical performance are some of the health irregularities that can occur. Nausea, vomiting and loss of appetite are further indications for an existing illness.
The complaints must be checked by a doctor so that a diagnosis can be made. A decrease in body weight, feelings of internal dryness, and restlessness should be presented to a doctor. Abnormal use of the toilet and bad breath are also among the health disorders that can be triggered by a duodenal ulcer. Changes in behavior, emotional irregularities and impaired digestion must be discussed with a doctor.
The affected person needs medical tests so that a diagnosis can take place. If left untreated, the existing ulcer continues to grow and can lead to numerous complications as well as a further decrease in health. Bleeding stool or discoloration of the stool are worrisome. If these peculiarities occur, there is a need for immediate action. A doctor's visit is necessary so that treatment can be initiated and the symptoms can be relieved.
Treatment & Therapy
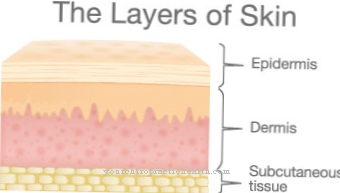
The basic therapy in the therapy of a Duodenal ulcer consists in effective acid inhibition. An attempt is made to restore the disturbed balance between damage and protection of the mucous membranes. In most cases, drugs from the group of active substances called proton pump inhibitors are used, e.g. Pantozole or omeprazole. In many studies, these show the strongest acid protection with comparatively few side effects.
Since there is usually a causal infection with Helicobacter pylori, the therapy is supplemented by two antibiotics (triple therapy) after the bacterium has been detected. Clarithromycin is standard, and amoxicillin or, alternatively, metronidazole is also used. Surgical therapy is now mostly only necessary for complications. As a rule, parts of the stomach are completely removed.
Typical indications are uncontrollable bleeding, a breakthrough of the duodenal ulcer or a suspected malignant tumor. Even if acid production cannot be effectively reduced with medication, it can be treated surgically by cutting through a nerve cord that regulates acid production.
In addition, nicotine and alcohol as well as spicy dishes should be avoided in the case of a duodenal ulcer. Stress reduction and a healthy, sporty lifestyle should also be aimed for.
Aftercare
In most cases, the person affected with a duodenal ulcer has very few and only very limited follow-up measures available, so that the person affected should ideally consult a doctor early on in this disease and initiate treatment. The sooner a doctor is consulted in the case of duodenal ulcer, the better the further course of this disease is usually.
Most of those affected are dependent on the intake of various medications that can relieve and limit the symptoms. The choice of medication depends heavily on the cause of the disease. In general, the person concerned should ensure that they are taken regularly and that the dosage is correct. If anything is unclear or if you have any questions, you should first consult a doctor so that there are no other complaints or complications.
When taking antibiotics, it should also be noted that they should not be taken together with alcohol. In general, if you have duodenal ulcer, it is also advisable to follow a healthy lifestyle with a balanced diet. Alcohol and nicotine should be avoided if possible. The disease itself can in some cases reduce the life expectancy of the person affected.
You can do that yourself
Duodenal ulcer A duodenal ulcer generally requires medical treatment. The highly effective medication usually brings about a rapid improvement, but various self-help measures can support the healing process. They also help prevent re-ulceration.
It is particularly important to consistently avoid the trigger. This applies not only to the acute phase of the illness, but also afterwards. The typical triggers of a duodenal ulcer are primarily alcohol, tobacco products, milk and foods containing sugar. But spices such as mustard, pepper and horseradish can also have a stimulating effect on acid formation. Certain drugs such as acetylsalicylic acid, which are not always necessary to take, are also problematic.
We recommend diets that are gentle on the mucous membrane, such as a tea and rusks diet for 24 to 36 hours. After that, the patient gradually returns to their usual diet. In the first two days, a light diet made from potatoes and cooked vegetables makes sense. From the third day onwards, low-fat meat dishes can be consumed again. It is also helpful to have several small meals a day instead of just a few large menus.
Relaxation methods such as meditation or autogenic training are another possibility for self-help. They are mainly effective against stress-related complaints. In addition, alternative treatment methods such as acupuncture or the use of homeopathic drugs such as Acidum sulfuricum, Nux vomica, Belladonna or Acidum muriaticum can be used.









.jpg)



.jpg)










.jpg)
