As Rothmund-Thomson Syndrome is called a genetic skin disease. It is inherited in an autosomal recessive manner.
What is Rothmund-Thomson Syndrome?

© logo3in1 - stock.adobe.com
The Rothmund-Thomson Syndrome (RTS) is one of the genetic skin diseases. In the face area in particular, pronounced poikiloderma occurs, which is associated with orthopedic and ophthalmological complaints. There is also an increased risk of developing certain cancers.
The name Rothmund-Thomson syndrome goes back to the description of two doctors. This took place for the first time in 1836 by the German ophthalmologist August von Rothmund (1830-1906). In 1936 the English doctor Matthew Sydney Thomson (1894-1969) published two papers dealing with hereditary poikiloderma (Poikiloderma congenitale).
This disease is the same as the diseases described by August von Rothemund. For this reason it was later named Rothmund-Thomson Syndrome. Rothmund-Thomson syndrome can be counted among the rare diseases. Until 2014, only 300 cases of illness were registered. The syndrome occurs in families, which is typical for hereditary diseases.
Blood relatives or small communities are primarily affected. There is a balance between the two sexes in terms of the number of diseases. Due to the low number of cases, however, no precise information can be given. In addition, no particular ethnic group is particularly affected by Rothmund-Thomson syndrome. The carrier frequency of the mutation is not known.
causes
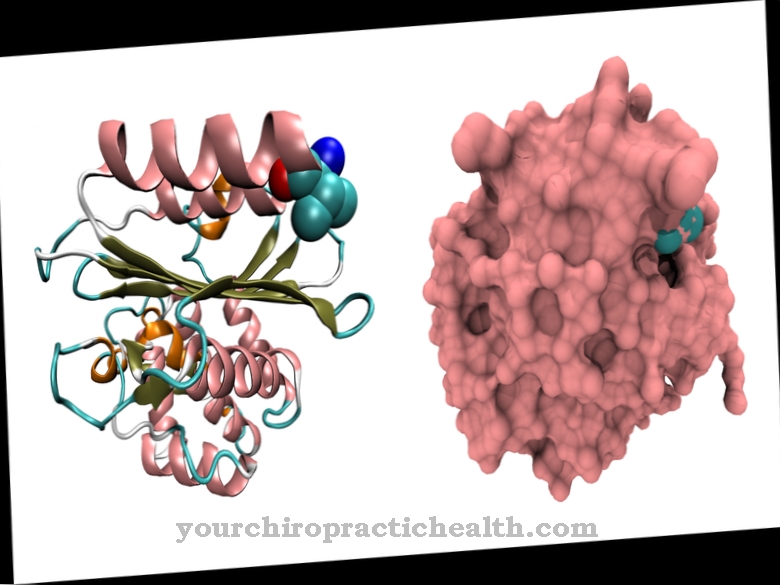
In medicine, Rothmund-Thomson syndrome is divided into the subforms RTS-1 and RTS-2. It has not yet been possible to clarify what causes RTS-1. RTS-2 can be traced back to a heterozygous mutation which originated in the RECQL4 gene. The affected gene is coded for a helicase.
The most common mutation is the nonsense mutation. In between 60 and 65 percent of all patients, defects in the RECQL4 gene are the cause of the development of Rothmund-Thomson syndrome. Both types RTS-1 and RTS-2 are inherited in an autosomal recessive manner.
Symptoms, ailments & signs
A typical feature of Rothmund-Thomsons syndrome is the unmistakable rash on the face, which is poikiloderma. This rash is the main symptom of the genetic skin disease. Poikiloderma also distinguishes the disease from the RAPADILINO syndrome.
Other characteristics of Rothmund-Thomson syndrome are sparse head hair, the frequent lack of eyelashes or eyebrows, short stature, skeletal malformations, adolescent cataracts and the occurrence of a radial club hand. Furthermore, the affected people age prematurely and develop a predisposition to cancer.
The symptoms vary between RTS-1 and RTS-2. In RTS-1, poikiloderma, ectodermal dysplasia and juvenile cataracts of the eyes occur. Patients with subtype RTS-2 also suffer from poikiloderma. In addition, there are congenital deformations of the bones and an increased risk of the occurrence of osteosarcomas, malignant bone tumors in adolescence. In further life it can also lead to skin cancer.
The malformations of the skeleton in Rothmund-Thomson syndrome are noticeable, among other things, by a saddle nose, a radial club hand or a prominent forehead. In some cases, however, they can only be detected by x-rays.
Diagnosis & course of disease
A distinction must also be made between the two forms of Rothmund-Thomson syndrome in diagnostics. No molecular genetic triggers could be found for the development of RTS-1. For this reason, the diagnosis is based on the symptoms present. A special evaluation table was created for this purpose, which is used to collect the various disease complaints.
With the help of point values, the examining doctor can determine whether RTS-1 is present. If RTS-2 is suspected, it is possible to determine the mutation in the RECQL4 gene by performing a genetic test. This usually also provides evidence of RTS-2. Rothmund-Thomson syndrome should be considered if patients have osteosarcoma. A differential diagnosis must be made for RAPADILINO syndrome and Baller-Gerold syndrome, as mutations in the RECQL4 gene can also be found in these diseases. The Rothmund-Thomson syndrome takes a different course.
Despite their visible premature aging process, the patients have a relatively normal life expectancy, provided there is no malignant cancer. Some patients are at increased risk of developing secondary malignancies. In these cases, the prognosis depends on the quality of cancer screening and cancer treatment. If osteosarcomas occur, the 5-year life expectancy of patients is between 60 and 70 percent.
Complications
In Rothmund-Thomson syndrome, people suffer from a number of different skin conditions. These complaints have a very negative effect on aesthetics, so that many sufferers feel uncomfortable and suffer from inferiority complexes or from a reduced self-esteem. Depression or other psychological complaints can also occur as a result. Rothmund-Thomson syndrome can lead to bullying or teasing, especially in children.
Furthermore, there is also a short stature and various malformations on the skeleton. The patients suffer from restricted mobility and in some cases from the development of bone tumors. Skin cancer can also develop as a result of the disease and may significantly reduce the life expectancy of the person affected. Furthermore, in many cases the parents or relatives are also affected by the symptoms of Rothmund-Thomson syndrome and also suffer from psychological complaints.
Since there is no causal treatment for the syndrome, only symptomatic treatment can be carried out. There are no complications. However, those affected depend on stem cell transplants to defeat the cancers. As a rule, a completely positive course of the disease cannot be achieved.
When should you go to the doctor?
Since Rothmund-Thomson syndrome is a hereditary skin disease with a familial prevalence, contacts with a doctor are inevitable at the beginning of life. However, the poikiloderma in the facial area associated with the disease is not the only symptom that makes life difficult for those affected.
People with Rothmund-Thomson syndrome also suffer from orthopedic or ophthalmological complications. People of both sexes are also more likely to develop cancer. The two subtypes of Rothmund-Thomson syndrome, however, occur comparatively rarely. No more than 300-320 cases are documented in the world.
Given the rarity of Rothmund-Thomson syndrome, it is comparatively difficult to find a specialist doctor who can diagnose Rothmund-Thomson syndrome. Differentiation from other syndromes with similar symptoms is necessary. Medical treatments are indispensable in most cases, even if there is no chance of a cure. Rothmund-Thomson syndrome can only be treated symptomatically. Specialists and specialists from various disciplines will strive for close cooperation.
The cooperation of dermatologists, orthopedists, ophthalmologists, surgeons or oncologists is the best way to help those affected achieve a better quality of life.
Therapy & Treatment
There is currently no therapy for the cause of Rothmund-Thomson syndrome. For this reason, treatment is limited to relieving symptoms. Since the symptoms are extremely complex, it is advisable to have the patient treated on an interdisciplinary basis. This means that the therapy is carried out by doctors from different specialties. In the case of Rothmund-Thomson syndrome, this includes surgeons, orthopedists, ophthalmologists, oncologists and dermatologists (dermatologists).
Symptomatic therapy includes an annual ophthalmological examination, treatment of telangieectasias, and radiological examinations to control osteosarcomas. Stem cell transplantation is a possible new therapy option. It is still in clinical trials and has only been performed on two patients so far. One patient underwent allogeneic bone marrow transplantation. In the other case, treatment was carried out using umbilical cord blood stem cells.
You can find your medication here
➔ Medicines against redness and eczemaprevention
Unfortunately, it is not possible to take preventive measures against the outbreak of Rothmund-Thomson syndrome. The condition is one of the hereditary diseases, the cause of which is still largely unknown.
Aftercare
Follow-up care for Rothmund-Thomson syndrome depends on the subtype of the disease and its course as well as the treatment measures chosen and the patient's constitution. In general, follow-up will review the various symptoms and discuss the next steps. Surgical intervention often places a significant burden on the patient.
During the follow-up, the surgical scars are checked to determine the success of the treatment. Furthermore, the patients are encouraged to rest. Treatment with painkillers may be necessary for protracted illnesses. In addition, patients sometimes need psychological support. Part of the follow-up care is also the education about advances in novel therapy methods such as stem cell transplantation or bone marrow transplantation, which have so far been successfully carried out in some patients.
In addition, the follow-up includes a routine examination of the various physical functions that have been affected by the cancer. If no complications arise, the patient can then be discharged. Since this is an extremely rare condition that can only be treated symptomatically, close medical monitoring is advisable for the patient even after recovery. Follow-up care for Rothmund-Thomson syndrome is carried out by a dermatologist, orthopedist, ophthalmologist, oncologist or surgeon, depending on the symptoms.
You can do that yourself
Since Rothmund-Thomson syndrome is associated with an increased risk of cancer, the person affected should independently examine their body for irregularities or abnormalities in the skin at regular intervals. In addition to medical visits for medical examinations, it is advisable to seek the help of other people in everyday life to clarify areas that are difficult to access for possible changes in the skin's appearance.
Since the genetic disease already shows abnormalities in the first years of life, the growing child should be informed about the existing disease and its further course at an early stage. In dealing with the disorder on a daily basis, it is important to avoid sudden situations and unpleasant surprises. Therefore, the close social environment should also be informed about the existing health impairment. Since there are visual changes, it is important to strengthen self-confidence in the child's development and growth process.
Since surgical interventions are often used to improve the situation, mental support for the child is just as important as strengthening the immune system. In order to cope with an operation, the organism needs defenses. Mental strength can be built up in collaboration with a psychotherapist. In addition, the therapies offered help to be able to process the challenges of the disease emotionally well. In some cases, parents should also consider seeking psychotherapeutic treatment.

.jpg)
.jpg)






.jpg)

.jpg)
.jpg)











.jpg)