The Acinetobacter are a group of bacteria from the genus Gammaproteobacteria, all of which are gram-negative and encompass many different forms of life. Acinetobacter is one of the best-known aerobic bacteria and is primarily known as a multi-resistant hospital germ. Infection can be fatal for immunodeficient patients.
What are Acinetobacter?

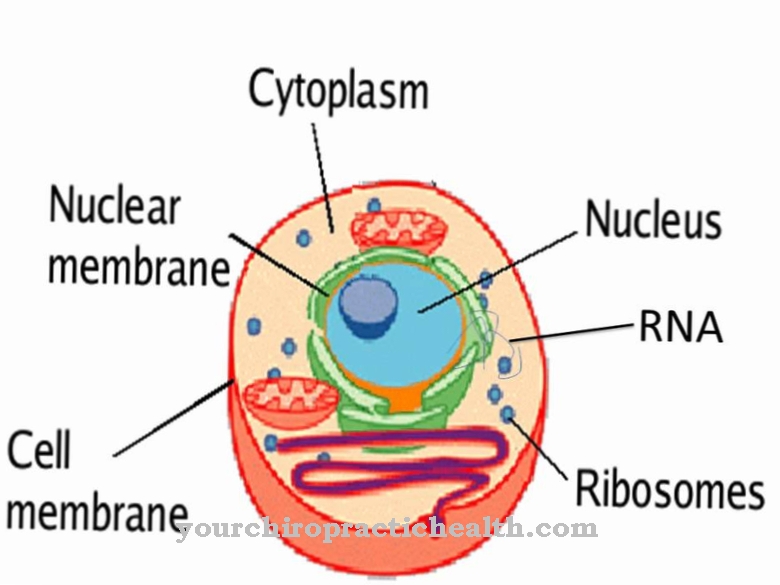
Gammaproteobacteria are also referred to as γ-Proteobacteria. It is a class of the phylogenetic bacterial system. This system was set up on the basis of the base sequence of 16S ribosomal ribonucleic acid, also known as 16S rRNA. The strain of the Proteobacteria contains 5 classes from Alphaproteobacteria to Epsilonproteobacteria. Every single representative from this bacterial strain is gram negative. Gammaproteobacteria are the most species-rich class from the Proteobacteria group and are physiologically extremely diverse.
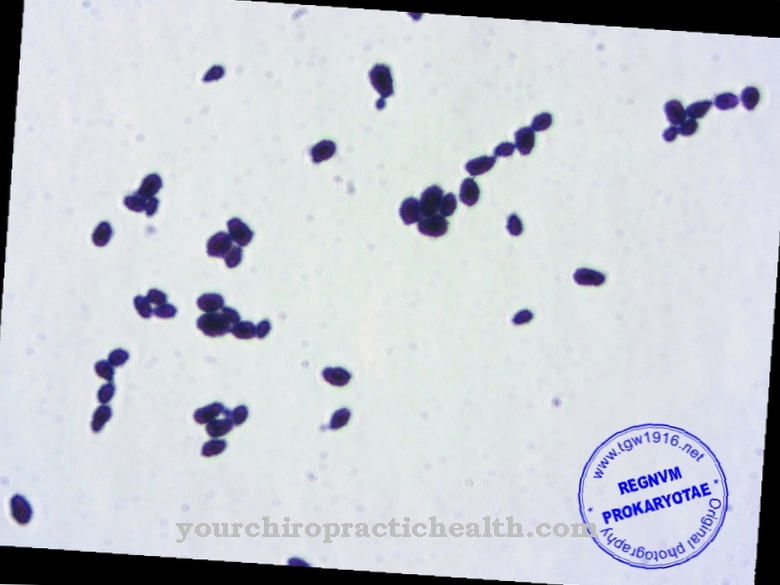
Bacteria of the genus Acinetobacter also belong to the gramaproteobacteria. They are gram negative and are considered one of the most common types of bacteria. In most cases, the bacteria are multi-resistant and can therefore cause serious diseases that cannot be treated conventionally. Acinetobacter baumannii, for example, is pathogenic to humans and therefore always associated with disease value in humans. Due to its resistance, this germ is one of the most feared germs worldwide. The germ is one of the most common hospital germs. Other species from the genus are Acinetobacter johnsonii, junii, lwoffii and Acinetobacter towneri. A total of around 20 species are known from the group.
Occurrence, Distribution & Properties
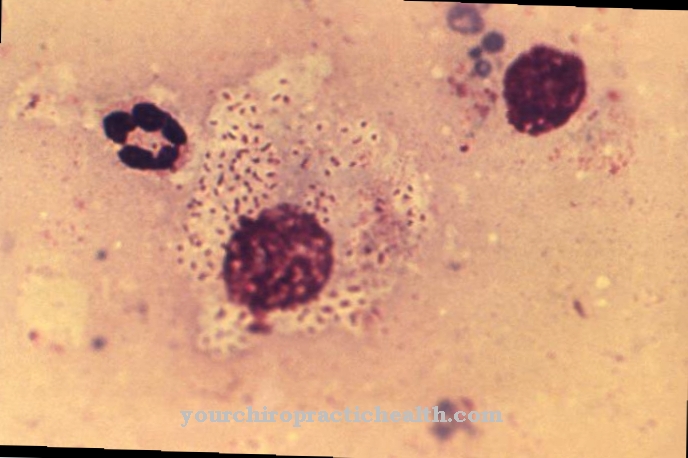
Acinetobacter baumannii bacteria are aerobic short-rod bacteria. The type of bacteria needs oxygen to survive and is therefore one of the aerobic bacteria. This is what sets it apart from most other types of bacteria. Many of them do not necessarily need oxygen or even experience oxygen as lethal. From a chemical point of view, aerobics is characterized by oxidation. So if the individual processes within the bacterial organisms use oxygen, we are talking about aerobic organisms. Acinetobacter baumanii cannot survive without oxygen.
In addition, it is one of the short-rod bacteria. Species that are shorter than twice their width are designated as such. The bacteria of the species Acinetobacter baumanii are also so-called environmental germs, whose preferred habitat is the interior of the soil and the water. Acinetobacter baumanii often also colonize human skin. In this context, they also occur on the skin of healthy people. However, this colonization is to be understood as temporary, since healthy human skin is colonized by various skin bacteria. These naturally occurring bacteria on the skin create an unfavorable environment for Acinetobacter baumanii.
The spread of bacteria in the human body is therefore only possible under certain circumstances. An infection with Acinetobacter baumannii therefore usually affects people with severely weakened immune systems. The infection is classified as a nosocomial infection, since it appears to occur more frequently during hospital stays. An infection is not necessarily the case after contact with the germ. For healthy people, the contacts usually have no consequences, as their immune system kills the bacteria in time. Since the bacteria cannot multiply sufficiently before the rapid intervention of a healthy immune system, no symptoms occur.
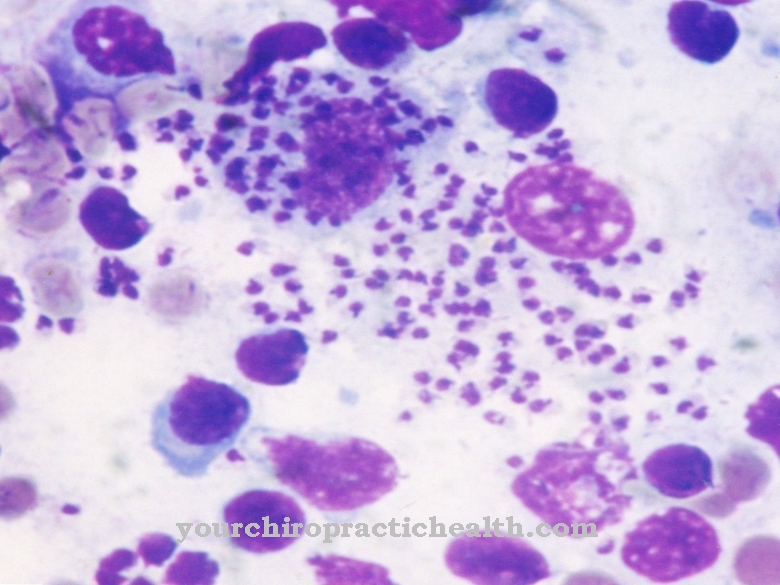
In people with a weakened immune system, such as AIDS patients or consciously immunosuppressed patients (e.g. after an organ transplant), the immune system does not intervene quickly enough. The germ can reproduce by dividing and spreads through the bloodstream. An infection develops. The bacteria of this species especially colonize wounds or organs such as the lungs due to their environmental preferences.
Illnesses & ailments
Acinetobacter baumanii can cause serious wound infections and pneumonia in immunosuppressed or otherwise immunocompromised people. The most serious complication of these phenomena is sepsis. This is an inflammatory reaction of the entire organism, which is also known as blood poisoning and can be fatal.
Other types of Acinetobacter cause meningitis, especially Acinetobacter lwoffii, junii, haemolyticus and johnsonii. In this context, the pathogens spread to the brain via the bloodstream.
While drugs can help against other Acinetobacter species, Acinetobacter baumannii are multi-resistant. A multi-resistant strain was first reported in the Dutch intensive care unit at the Enschede Clinic. In 2015, there was also talk of a multi-resistant strain at the Kiel University Hospital after 31 patients were infected with Acinetobacter baumannii. The strain was classified in the 4-MRGN group: none of the four groups of antibiotics could harm the bacterium. The infection led to death in 12 cases. At the end of 2015, the Linz Women's and Children's Hospital reported a germ of the Acinetobacter species that had infected a total of five babies, three of whom died.
The use of broad spectrum antibiotics is now suspected by science as the main reason for the increased occurrence of Acinetobacter. According to the Robert Koch Institute, the multi-resistant proportion of strains rose to 10.7 percent between 2009 and 2011. Multi-resistances arise on the basis of the evolutionary adaptability and learning ability of bacteria. Usually at least one of four groups of antibiotics is initially effective against the germs. However, the more often they come into contact with the medication, the faster they develop resistance to the relevant active ingredients. We only speak of multi-resistance if a bacterium has already become resistant to several active substances.








.jpg)


.jpg)

.jpg)