Osteocalcin is a peptide hormone found in bones with various functions. It is significantly involved in bone metabolism and serves as a marker for various bone diseases in the blood. But it also plays a major role in the metabolism of carbohydrates and fats.
What is osteocalcin?
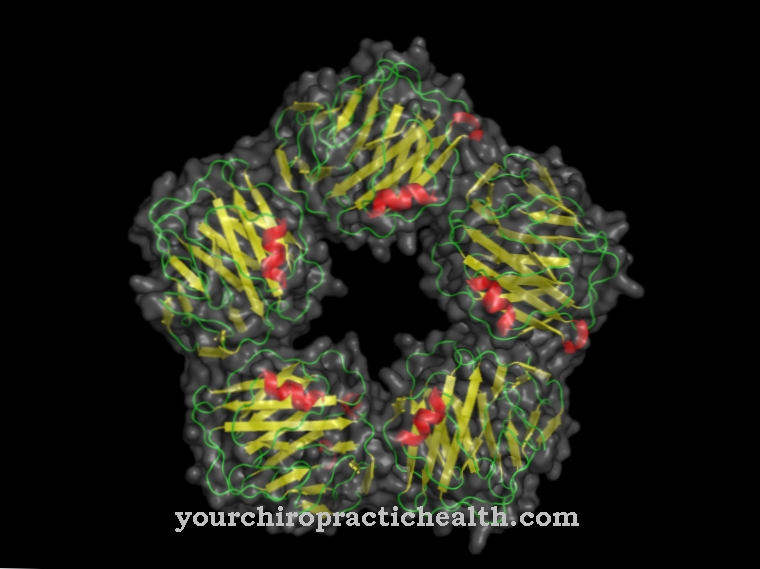
Osteocalcin is a peptide hormone which is produced in the osteoblasts of the bones or the odontoblasts of the teeth. As part of the extracellular bone matrix, it binds to the mineral hydroxyapatite. There it is about one to two percent.
Due to the binding to the calcium of the mineral, osteocalcin inhibits the uninhibited mineralization of the bone. It is encoded by a gene on chromosome 1q25q31. In studies on mice, mutations in this gene led to increased mineralization of the bones and thus to the development of marble bone disease. This resulted in increased bone formation and, at the same time, increased fragility. The synthesis of the hormone depends on the vitamin D metabolite calcitriol (1,25 (OH) 2D3).
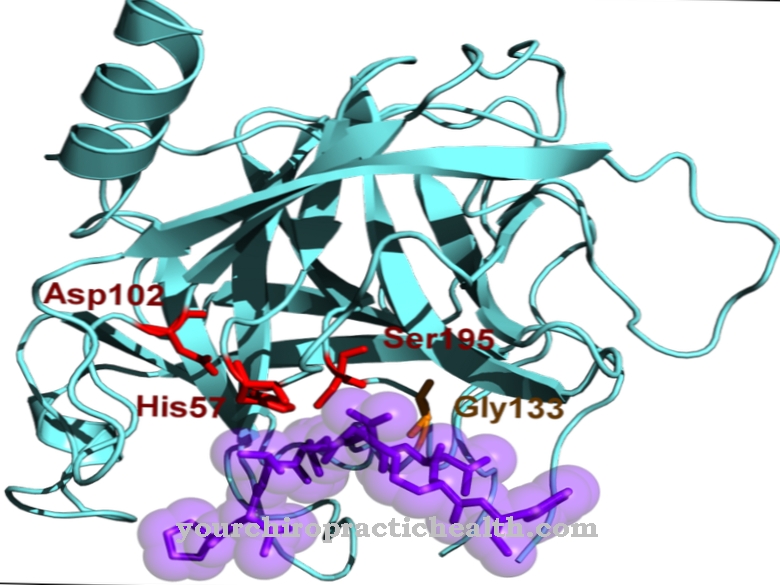
The binding to calcium is in turn catalyzed by the enzyme glutamyl carboxylase. Vitamin K acts as a cofactor. Osteocalcin acts as a marker of bone structure. It has already been isolated from surviving Neanderthal bones. It is measured in the blood for diagnostic purposes.
Function, effect & tasks
Osteocalcin fulfills several functions in the organism. It is a hormone that is only synthesized in the osteoblasts of the bones or the odontoblasts of the teeth.
There it is significantly involved in bone metabolism. Bone-building and bone-degrading processes are constantly taking place within the skeletal system. If the bone-degrading processes predominate, what is known as osteoporosis occurs. While the hormone does not prevent osteoporosis, it does act as an important marker for certain bone diseases. Within the bone, its job is to limit the mineralization of the bones. It binds to the hydroxyapatite of the extracellular non-collagenous bone matrix. The bones develop normally and are given the necessary strength against fractures. The matrix contains up to two percent. In order to be able to bind to the calcium atoms of the mineral, the glutamyl residues contained in osteocalcin must first be removed with the help of an enzyme.
This enzyme is glutamyl carboxylase, which in turn is activated with the cofactor vitamin K. According to the latest findings, osteocalcin also lowers blood sugar and reduces fat. The blood sugar lowering comes about in two ways. Osteocalcin stimulates the synthesis of the hormone insulin directly by stimulating the islets of Langerhans in the pancreas. It also indirectly increases the effectiveness of insulin by stimulating the hormone adiponectin. In recent years it has been found that [[insulin resistance is caused by a reduced production of adiponectin.
The more fat is stored in the adipocytes, the lower the adiponectin synthesis. This in turn reduces the effectiveness of the insulin. In addition, animal experiments have shown that osteocalcin boosts fat burning. Mice with high levels of osteocalcin did not develop obesity or diabetes. Based on this research, future approaches could emerge to combat obesity and type II diabetes more effectively with the help of osteocalcin.
Education, occurrence, properties & optimal values
As mentioned earlier, osteocalcin is synthesized in the osteoblasts of the bones and in the odontoblasts of the teeth. Its production rate depends on vitamin K and is stimulated by vitamin D. After its formation, it is then mainly incorporated as a component in the extracellular bone matrix. Only there is it stable.
In free form it has only a short half-life. In the blood plasma, for example, it is half broken down by the proteases it contains within four minutes. It is released during bone turnover and gets into the blood. The measured concentrations in blood and urine provide information about the metabolic activity of the bones and are therefore a good marker for certain bone diseases.
Diseases & Disorders
The levels of osteocalcin in the blood and urine depend on many factors. In general, they characterize the bone turnover rate. During bone turnover, bones are constantly broken down and rebuilt.
When the bone-degrading processes predominate, the bone density decreases in the long term and the fragility increases. Of course, more substances are released that are involved in bone formation. This also includes osteocalcin. High values in the blood always mean increased breakdown processes. Too high osteocalcin levels in the blood are found in osteoporosis with a high metabolic rate, hyperparathyroidism, bone metastases in malignancies, Paget's disease, osteomalacia, hyperthyroidism or renal insufficiency. Low osteocalcin levels occur with prolonged corticosteroid therapy, osteoporosis with low bone turnover, rheumatoid arthritis or hypoparathyroidism. Osteoporosis in particular can be caused by many different causes. Therefore, bone turnover can be high or low.
What all forms of osteoporosis have in common is that bone loss predominates over bone structure. Hormonal disorders based on an overactive parathyroid hormone cause the osteocalcin levels in the blood to rise sharply. The parathyroid hormone regulates the level of calcium in the blood by breaking down the bones. Conversely, too low parathyroid hormone concentrations also lead to low osteocalcin values in the blood. In the context of Paget's disease, irregular remodeling processes occur in the skeletal system, which also leads to increased osteocalcin concentrations.
Of course, with generally increased metabolic rates in the context of an overactive thyroid, bone turnover increases with increased osteocalcin levels. Cortisone therapy slows bone turnover. The blood values are typical for certain diseases. However, the determination of osteocalcin provides only one result in the context of the overall diagnosis.

.jpg)







.jpg)

.jpg)
.jpg)











.jpg)