The Acrogeria is also as Gottron Syndrome known and characterized by a complex of predominantly dermal symptoms such as atrophy and telangieectasia. The disease is based on a mutation in the COL3A1 gene that disrupts the biosynthesis of type III collagen. So far, therapy has been purely symptomatic.
What is acrogeria?

Endocrine disorders group of diseases includes various diseases that affect the glands. Acrogeria, better known as Gottron's syndrome, is also included in the group of congenital, endocrine disorders. The main symptom of this disease is the atrophy of the skin and subcutaneous adipose tissue, which gives the patient a pre-aged appearance.
The Gottron acrogerie was first documented in 1940. The German dermatologist Heinrich Gottron is considered to be the first to describe the disease. Women are more often affected by the disease than men. The ratio is about three to one. Therefore, in connection with the Gottron acrogeria, gynecotropy is mentioned. The prevalence of the syndrome is not yet known. It is estimated to be an extremely rare phenomenon. The disease is apparently a hereditary disease and manifests itself in infancy. Usually there is talk of a manifestation immediately after birth.
causes
The cause of Gottron syndrome lies in genetics. The disease does not appear to be sporadic. Family clusters have been documented in connection with the syndrome. The inheritance is apparently based on an autosomal recessive inheritance. However, due to its rarity, the inheritance of the disease is not considered to be undoubtedly certain. It is possible that inheritance can also take place in an autosomal dominant mode of inheritance.
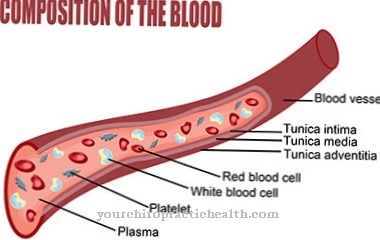
A genetic mutation is what causes the symptoms. The mutation has now been localized to a specific gene. Those affected usually have a mutation in the COL3A1 gene at locus 2q32.2. The COL3A1 gene codes in the DNA for the pro-alpha1 chains of type III collagen. Type III collagen is found in the skin as well as the lungs, blood vessels and the gastrointestinal tract.
The mutation appears to cause a disruption in the biosynthesis of type III collagen, which favors acrogeria. Other sources suspect that the LMNA gene at locus 2258301 is also involved.
You can find your medication here
➔ Medicines against skin redness and eczemaSymptoms, ailments & signs
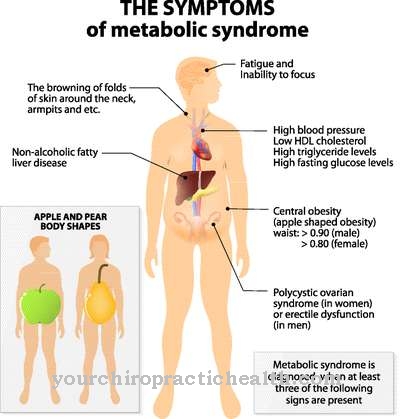
Acrogeria patients suffer from a complex of various clinical symptoms, most of which affect the skin. One of the most important criteria of acrogeria is its manifestation in infancy or early toddler age. The patients suffer from acromicria or micrognathia with profound atrophy of the skin and subcutaneous tissue. The underlying structures are extremely contoured.
In most cases, patients are prone to injury and often suffer from telangieectasias. In many of those affected, these symptoms are associated with facial erythema. The skin of the face is usually atrophic and therefore looks wilted. Scarlet-like rashes are an equally common characteristic.
Patients' nails are often affected by dystrophy. In individual cases the symptoms of acrogeria are associated with those of scleroderma. In these cases, sclerosis and fibrosis of the connective tissue can round off the clinical picture. The growths are benign and usually do not tend to degenerate.
Diagnosis & course
The diagnosis of acrogeria is made in most cases postnatally or in infancy. The pre-aged appearance and general clinical picture of the patients arouses the first suspicion of the disease. Imaging is usually initiated for diagnosis. The x-ray of the patient shows a rarefaction of cancellous bone.
In many cases there is also a missing closure of the epiphyseal plates. Diseases such as Brugsch syndrome, Hutchinson-Gilford syndrome, aplasia cutis congenita and Ehlers-Danlos syndrome are to be distinguished from the differential diagnosis. The demarcation from the latter syndrome is a particular challenge for the doctor.
While the other diseases can be differentiated within the framework of a molecular genetic analysis, this is not easily possible with Ehlers-Danlos syndrome. Like acrogeria, this syndrome is based on a mutation in the COL3A1 gene. The prognosis for patients of acrogeria is this Cheap.
Complications
Acrogeria causes various complications in its course, which mainly affect the skin. Patients are prone to injuries to the face and the whole body, which are often inflamed and lead to permanent skin changes or secondary diseases. Scarlet-like skin rashes are typical, which can lead to bleeding, pigmentation disorders or sensory disorders.
The changes to the skin also cause visual changes that can cause psychological problems such as inferiority complexes or fears in those affected. Acrogeria in the nail area can be associated with sclerosis or fibrosis. Corresponding growths, however, are usually benign and only temporarily lead to health restrictions.
The lower jaw, which is often smaller in acrogeria, can cause speech disorders and disorders in tooth development, but also breathing difficulties and even sleep apnea. When treating acrogeria, the prescribed medication can aggravate the symptoms. If this is accompanied by an allergy or intolerance, in severe cases this can lead to organ failure and ultimately to death of the patient. By clarifying the acrogeria at an early stage, suitable therapeutic measures can be initiated and serious complications can usually be avoided.
When should you go to the doctor?
Since acrogeria mainly causes discomfort on the skin and face, these should always be treated by a doctor. They appear in childhood and can therefore be identified and diagnosed quite easily. In general, skin conditions in children should always be examined by a doctor to rule out serious illnesses. In acrogeria, the doctor should be consulted if there are growths on the face or body.
Even if these are benign in most cases and primarily do not pose a health risk, they should still be treated. It is not uncommon for acrogeria to lead to inferiority complexes or to reduced self-esteem. A visit to a psychologist is recommended to prevent depression or other psychological upsets later on. Bleeding or pigmentation disorders can also be a sign of acrogeria.
Not infrequently, the drugs used to treat acrogeria also lead to severe side effects and, in the worst case, to organ failure. If this leads to symptoms or strange feelings, a doctor must be consulted. In this case, after consulting the doctor, the drug can either be discontinued completely or replaced with another drug.
Doctors & therapists in your area
Treatment & Therapy
Causal treatment is not available for acrogeria patients. Causal therapy will only be possible once gene therapy steps have been approved. So far, however, these treatment measures have not reached the clinical phase. For this reason, acrogeria has so far been considered an incurable disease. The therapy is purely symptomatic and thus depends on the symptoms in the individual case.
For example, the atrophy must be slowed down or brought to a standstill by targeted measures. A progressive breakdown of tissue should be prevented by blood-stimulating drugs and stimulating the metabolism. Malformations such as micrognathia can be corrected surgically. The same is true for symptomatic fibrosis.
One of the most important therapy steps is physiotherapy treatment, which both stimulates the metabolism and can reduce accompanying symptoms such as telangieectasias. In addition to sporting activities, dietary measures can reduce the symptoms of acrogeria. Because of their rarity, little is known about the effectiveness of individual treatment steps.
There are hardly any informative case reports or clinical studies on specific treatment options. In connection with atrophy and telangieectasia, however, a combination of exercise and a healthy diet has proven successful in the past.
Outlook & forecast
Acrogeria usually causes discomfort on the skin. These can occur either on the face or on the rest of the body and thus always lead to unpleasant complaints. In most cases, psychological discomfort also occurs, as acrogeria has a negative effect on the patient's appearance. In some cases, inferiority complexes develop and self-esteem is reduced. Sometimes the patients are ashamed of the symptoms and are socially excluded.
Often the patients generally feel sick and exhausted and no longer actively participate in life. Those affected can also suffer from pigment disorders, which, however, do not pose any particular health risk to the patient. In some cases, the use of certain medications can exacerbate acrogeria, and in the worst case this can also lead to death if organ failure occurs. The disease is currently only treated symptomatically and can limit many symptoms. However, no general prediction about the course of the disease is possible.
You can find your medication here
➔ Medicines against redness and eczemaprevention
Acrogeria is a genetic disease that is based on mutations. So far, the involvement of any external factors is still unclear. Because of these relationships, no preventive measures are available.
You can do that yourself
Acrogeria must always be diagnosed and treated by a doctor first. In addition to medical therapy, the individual symptoms of the disease can be alleviated by various measures.
Physiotherapeutic treatment is particularly recommended, which stimulates the metabolism and alleviates possible accompanying symptoms such as telangiectasias. In addition, dietary measures can alleviate the symptoms. Those affected should ensure a balanced diet with all the necessary vitamins and minerals. In addition, exercise and the avoidance of stress are recommended. Physiotherapy and yoga are particularly suitable for alleviating the typical symptoms and at the same time reducing the physical tension associated with the disease.
The typical skin changes can also be reduced with the help of care products from the pharmacy and various home remedies. However, visual changes usually remain, which should be worked up in a therapeutic consultation. If acrogeria has already developed inferiority complexes or fears, further psychological measures must be taken. Conversations with family members and friends can help to work through the manifold symptoms of the disease and to improve general well-being in the long term.










.jpg)

.jpg)
.jpg)











.jpg)