In the holocrine secretion gland cells themselves become part of a secretion by perishing during secretion. Such a mechanism occurs in the human organism in the secretion of sebum. Both overproduction and underproduction of sebum can be pathological.
What is holocrine secretion?

Holocrine secretion is a mode of secretion by exocrine secretion glands. In addition to holocrine secretion, the human organism has the modes of apocrine and eccrine secretion.
The release of holocrine secretions is found, for example, in human sebum glands. The holocrine secretion mode of the sebum glands is particularly popular in connection with apoptosis, i.e. programmed cell death.
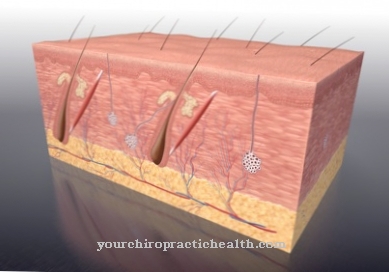
The secreting cells themselves become secretions during holocrine secretion and completely disintegrate during secretion. They are replaced by regrowing gland cells that advance towards the gland lumen. This advancement of new cells removes the old gland cells so far from the basement membrane that they can no longer be adequately nourished. As a result, they degenerate, lose contact with the surrounding cells and are rejected. It is only from the disintegrated membrane and the contents of the cells that the greasy-looking and actual secretion emerges.
Function & task
The holocrine secretion can be traced in detail using the example of the sebum glands. The sebum is formed intracellularly by so-called sebum cells. Several sebum cells are located in the interior of each sebum gland. Only when the individual cells burst open does the sebum reach the surface of the skin. The sebum contains triglycerides as well as wax esters and fatty acids.
Each sebum wall resembles the epidermal basal cell layer. It is equipped with a germ layer on which new sebum-producing cells are constantly forming. Regeneration of the epithelium takes place permanently from the basal cell layer. Some of the cells remain in the form of stem cells near the basement membrane. The other part is shifted by the subsequent cells, loses contact with the membrane and migrates towards the lumen. The further the cells are moved, the less diffusion-based nutrition can take place.
The sebum cells migrate to the middle of the gland and continuously produce fats. The lipids are collected and stored by the cell. Lipid droplets form on the surface and connect the migrating sebum cells with one another. As soon as a sebum cell reaches the center of the gland, it gradually perishes due to the stored fats and the nutritional situation. This creates a kind of sebum paste from the fats together with the cell components of the burst sebum cell. When this pulp pushes through the exit of the follicle onto the surface of the skin, the horny cells of the follicle wall are torn off and migrate out onto the skin together with the sebum pulp.
How much sebum is produced daily in this way is determined by the disposition and the hormones. Age, nutritional status and various environmental influences can also affect sebum production. The average daily production is one to two grams per day. Without the sebum or holocrine secretion, the surface of the skin would dry out.
Holocrine secretion is only produced by the sebum glands in the human organism. The large, branched alveolar sebum glands of humans are mostly located on hair shafts. The small, single alveolar sebum glands lie on the skin. Meibohm's glands are the well-branched and alveolar sebum glands on the eyelid and the small sebum glands on the eyelashes are also known as Zeiss glands.
Illnesses & ailments
The holocrine secretion of the sebum glands can be disturbed by various diseases. As a rule, impaired sebum administration becomes noticeable in the form of skin diseases or at least abnormalities on the skin. If there is excessive holocrine secretion, it is also called seborrhea. This phenomenon can be symptomatic in the context of Parkinson's disease, acromegaly or phenylketonuria and thyrotoxicosis. The skin becomes abnormally oily.
A special form of the phenomenon is the disturbed secretion due to a sebum gland that is closed by overproduction. With this phenomenon, a so-called sebum build-up occurs after a certain time. The pores of the skin expand and thus offer pathogens the best possible entry points. In addition, the sebum build-up promotes the formation of blackheads. This phenomenon occurs, for example, in the context of acne.
It is to be distinguished from a reduced holocrine secretion, as suffered by sebostatics. Your skin becomes cracked and abnormally dry. Inflammation of the sebum glands can also have an impact on functionality and thus on holocrine secretion. Such inflammatory reactions are referred to as sebadenitis, which occurs rarely in humans and can lead to irreversible damage to the holocrine glands. As an idiopathic disease, sebadenitis and its causes have not yet been conclusively researched. A genetic cause is currently suspected.
An equally rare phenomenon is sebum carcinoma. In this malignant cancer, the cells from which the sebum glands were supposed to form degenerate.
A common disease of the sebum glands in the eye is stye, also known as the hordeolum. This phenomenon is usually bacterial and causes a painful inflammation, which manifests itself in reddening and swelling of the eyelid.












.jpg)
.jpg)
.jpg)







.jpg)