A antibiotic-associated colitis is a severe colitis caused by the bacterium Clostridium difficile that occurs after antibiotic treatment. The cause of this is damage to the intestinal flora. Under certain circumstances, the disease can develop into a fulminant course with a fatal outcome.
What is antibiotic-associated colitis?

© olenka758 - stock.adobe.com
After antibiotic treatment, severe antibiotic-associated colitis can occur if the intestinal flora is severely damaged. As a result, the ubiquitous Clostridium difficile bacterium multiplies in the intestine because the competing and vital bacterial strains of the healthy intestinal flora have been reduced. Antibiotic-associated colitis is also called pseudomembranous colitis designated.
The disease can break out four weeks after stopping antibiotic treatment. However, not all diarrhea after this treatment is caused by Clostridium difficile. Diarrhea often occurs during or after treatment with antibiotics, but this is usually very mild. In the majority of cases, this is a functional, self-limiting diarrhea that is triggered by a slight disturbance of the intestinal flora.
In 10 to 20 percent of cases, however, pseudomembranous colitis due to Clostridium difficile occurs and in very rare cases a very severe antibiotic-associated hemorrhagic colitis develops. The antibiotic-associated hemorrhagic colitis is caused by another bacterial strain, Klebsiella oxytoca. However, when antibiotic-associated colitis is mentioned, it is usually pseudomembranous colitis caused by Clostridium difficile.
causes
As already mentioned, the cause of the development of antibiotic-associated colitis is an infection of the intestine with the bacterium Clostridium difficile after antibiotic treatment. If the healthy intestinal flora is destroyed in the process, ideal growth conditions can arise for this bacterium. Clostridium difficile is not a necessary component of the physiological intestinal flora, but occurs in three to seven percent of cases in adults and up to 50 percent of cases in newborns.
In combination with the normal intestinal flora, however, there are no diseases. If the healthy flora of the intestine is destroyed, Clostridium difficile causes severe intestinal inflammation in some patients. The reason for the severe course of the disease is to be found in the fact that Clostridium difficile develops strong toxins which lead to severe inflammatory processes in the intestinal mucosa.
The bacterium secretes the two poisons toxin A and toxin B. Under the action of these toxins, explosive fibrin exudations occur in the intestine, which appear like cats' heads during the colonoscopy. The toxins of the bacteria are released when it is destroyed during the immune reaction. Against the poisons there are now repeated immune reactions. This explains the severe course of the disease.
You can find your medication here
➔ Medication for diarrheaSymptoms, ailments & signs
The main symptoms of antibiotic-associated colitis are severe diarrhea and abdominal cramps. Life-threatening complications can result, possibly leading to a toxic megacolon and organ failure. However, the severity of the disease also depends on how toxic the toxin excreted by the bacterium is. Constant genetic changes can result in both very virulent and less dangerous strains.
Should it come to infection with highly toxic strains, very fulminant courses of the disease often occur, which can lead to death within a short time. In addition to the septic course caused by SIRS (Systemic Inflammatory Response Syndrome) with megacolon and general organ failure, the drastic loss of fluid due to severe diarrhea can also cause the colitis to be fatal. In other cases, the courses are mild to even asymptomatic.
Diagnosis & course
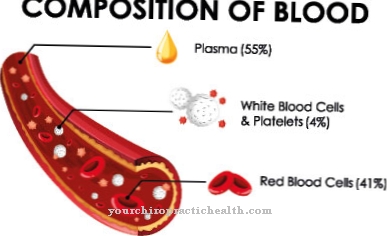
Antibiotic-associated colitis can be clearly diagnosed by detecting the pathogen and its toxins in the stool. Indications of the disease arise during the anamnesis from the temporal connection between antibiotic treatment and severe colitis. A clear indication is given if the diarrhea occurs within four weeks after therapy. The white blood cell count can reach very high values.
In imaging procedures such as ultrasound or computer tomography, an elongated intestinal thickening of the large intestine becomes visible. During colonoscopy, greenish fibrin coatings are discovered that appear spotty or flat.
Complications
In most cases, this disease causes severe gastric discomfort. The affected person suffers from very severe and frequent diarrhea and pain in the book and stomach. The quality of life is thereby reduced and normal activities are hardly possible for the patient.
In the worst case, this can lead to organ failure, which, however, occurs relatively rarely. Furthermore, the complications depend heavily on the toxin of the bacterium, which is why no general prediction is possible. The diarrhea can lead to severe fluid loss.
Treatment is primarily by replacing the antibiotic. There are no further complications and the course of the disease improves. The patient is also given infusions and plenty of fluids to counteract dehydration. Most of the time, the disease can be treated well so that the person is completely healthy again.
In severe cases or if treatment is started late, organ damage can result in death. Life expectancy is not affected by early treatment. There are no more complications or restrictions.
When should you go to the doctor?
In the worst case, this disease can lead to death. Therefore, a doctor should always be consulted when the symptoms and symptoms of this disease appear. As a rule, those affected suffer from very severe and painful cramps in the abdomen and also from diarrhea.
If these complaints occur for no particular reason, it is imperative to consult a doctor. Unfortunately, the symptoms are not particularly characteristic, so that the disease is often confused with common gastrointestinal flu.
In any case, a doctor must be contacted if the pain is severe and people may also lose consciousness. Internal pain in the organs can also occur. In acute emergencies, you should always go to a hospital or call an emergency doctor so that there are no further complications.
An initial examination in the event of slight complaints can, however, also be carried out by the general practitioner. As a rule, this disease can be treated relatively well with the help of antibiotics, so that there are no particular complications. For this, however, an early diagnosis is necessary.
Doctors & therapists in your area
Treatment & Therapy
To treat antibiotic-associated colitis, the first step is to suspend treatment with the offending antibiotic. The most common causative antibiotics for pseudomembranous colitis are clindamycin, aminopenicillins, cephalosporins and 3rd and 4th generation gyrase inhibitors. These antibiotics are replaced by metronidazole or, in very severe cases, vancomyzine.
At the same time, of course, the water and electrolyte balance is balanced by oral administration or infusions. After treatment, relapses occur in around 20 percent of cases. These are either due to new infections with or insufficient control of Clostridium difficile. After the first relapse, treatment is repeated with metronidazole or vancomyzine. However, if there is another relapse, the medication is administered over a longer period of time (seven weeks) in gradual doses.
Fidaxomicin has also recently been approved as a drug against Clostridium difficile. Another measure to prevent recurrences is the restoration of the physiological intestinal flora through a stool transplant. The stool of a healthy donor is stirred in physiological saline solution and transferred into the patient's intestine with the help of an enema.
Outlook & forecast
The prognosis of antibiotic-associated colitis depends on the strength of the immune system and the measures taken to build up the immune system.
In severe cases, the disease can be fatal as an internal breakdown occurs. The chances of getting relief from the symptoms decrease for people of old age, young children and with various pre-existing conditions. These have already weakened the organism and taken up natural resources of resistance that are no longer available.
Adults with an intact and stable immune system have a good chance of recovery. With an optimal lifestyle, healthy diet, sufficient exercise and the use of supplementary preparations to strengthen the body's own defense system, recovery is possible within a few days or weeks. If the intestinal flora is basically intact before taking the antibiotics, there are seldom further complications or delays in healing.
If you already have previous illnesses, the bowel function is impaired or the immune system is weakened. Delays in healing are possible and very likely. If the organism is exposed to harmful substances or germs, an immediate attack by pathogens can take place, which has far-reaching consequences. In these cases, the forecast prospects are to be classified as unfavorable. Organ failure threatens and the risks of permanent suffering or a threat to life increase immensely.
You can find your medication here
➔ Medication for diarrheaprevention
Since most cases of antibiotic-associated colitis occur in hospitals, hospital hygiene measures are necessary for their prophylaxis. This includes frequent hand washing and disinfection as well as quarantine measures for affected patients.
A person's intestinal flora is severely damaged by antibiotic-associated colitis. The clostridia in particular can then multiply strongly and trigger unpleasant to dangerous symptoms. The danger of dehydration is particularly precarious.
Aftercare
Follow-up care after the administration of antibiotics would be useful because the antibiotic-associated colitis can occur up to four weeks after discontinuation of the drug. However, this monitoring measure is often neglected. Antibiotics are prescribed relatively lightly today. The patient is then discharged without instructions on how to build up flora.
After prescribing antibiotics, he hardly ever has any follow-up care. This is particularly precarious because some antibiotics favor the development of antibiotic-associated colitis. The most important aftercare measure after a Clostridium difficile infection is to rebuild the damaged intestinal flora.
Close monitoring by the attending physician is useful after the acute treatment. It is known that at least a fifth of all patients suffer from a relapse after antibiotic-associated colitis. Either the clostridial infestation was not completely suppressed or a new colonization with clostridial took place.
In elderly patients, monitoring should be even more closely monitored after antibiotic-associated colitis. Elderly people have an increased risk of fulminant disease processes. A stool transplant often promises success after several relapses. Overall, follow-up care for antibiotic-associated colitis should be significantly improved.
You can do that yourself
Antibiotic-associated colitis cannot be influenced positively by the person affected. Only the fluid and electrolyte balance can be balanced by sick people in whom the disease takes a comparatively mild course. Sufficient rest and the removal of excretions if necessary must be encouraged.
A noteworthy alternative therapy measure is stool transplantation.In severe and recurring cases of antibiotic-associated colitis, a stool donation can often provide relief. The approach is that it is assumed that colonization of an intestine with healthy intestinal flora leads to the formation of a desirable intestinal flora again.
This therapy is straightforward and extremely successful. Essentially, the donor stool is mixed with saline and mashed. It can enter the body through an enema, a nasogastric tube, or capsules.
Any other measures that are supposed to rehabilitate the intestinal flora are not effective or are only effective to a limited extent. Taking probiotics and other drugs is usually pointless. Intestinal cleansing and similar procedures - especially those in which a substance is brought into the intestine - should under no circumstances be used in order not to further endanger the affected colon tissue.
Good personal hygiene can prevent re-infection by spreading the Clostridium difficile after healing.


.jpg)







.jpg)

.jpg)
.jpg)











.jpg)