Anticholinergics are widely used in medicine due to their effect in the parasympathetic nervous system. However, the side effects should not be underestimated.
What are anticholinergics?

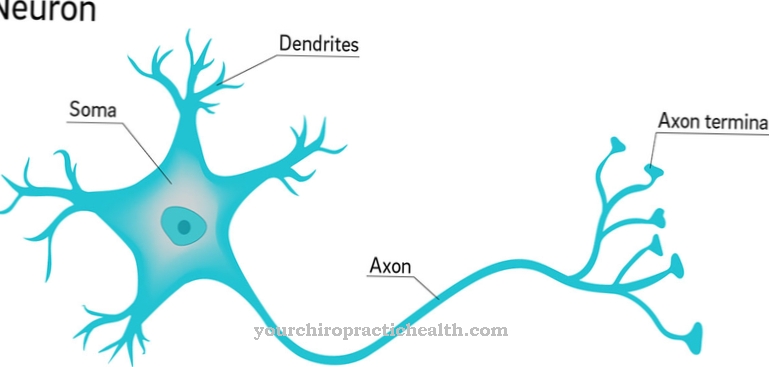
Anticholinergics are substances that inhibit the main carrier substance acetylcholine in the parasympathetic nervous system. As part of the vegetative (unconscious) nervous system and the antagonist of the sympathetic nervous system, the parasympathetic nervous system has the task of putting the body into a state of rest and regenerating.
The messenger substance acetylcholine is suppressed by interrupting certain nerve stimuli. Such nerve stimuli are responsible for the contraction of the smooth muscles and the secretion of the glands.
Acetylcholine thus stimulates the activity of the intestines and the digestive glands. In contrast, the heart rate and breathing decrease. Because of their effect in the parasympathetic nervous system, anticholinergics are also known as parasympatholytics.
Medical application, effect & use
The effects of the Anticholinergics on the human organism are a decrease in the flow of saliva, a dilatation of the pupils and a decrease in intestinal activity.
These modes of action result in various applications in medicine. Anticholinergics are used in particular for diseases of the irritable bladder. Patients with various types of incontinence and frequent urination experience a rapid improvement, as the anticholinergic substances weaken the contractions of the bladder muscles and thus increase the capacity of the bladder. The result of the more stable bladder is that those affected do not have to go to the toilet as often to empty their bladder.
Another important field of application for anticholinergics is Parkinson's disease, in which there is an excess of acetylcholine and a simultaneous lack of dopamine. Anticholinergic agents are administered to reduce this imbalance. Due to the numerous side effects, however, these are used cautiously and mainly to reduce the tremor in Parkinson's disease.
In addition, the drugs are effective for excessive sweating (hyperhidrosis), asthmatic diseases, bronchitis, cramps of the internal organs and smooth muscles, bradycardia (too slow heartbeat) and cardiac arrhythmias. In addition, anticholinergics are used to induce anesthesia prior to operations and to facilitate examinations of the fundus by dilating the pupils.
Herbal, Natural & Pharmaceutical Anticholinergics
The different types of Anticholinergics differ only slightly. However, there are differences with regard to tolerability.
In the event of intolerance, it is therefore helpful to change medication. There are two major groups of anticholinergics: the first group acts exclusively on the nervous system (neurotropic) and the second group acts both on the nervous system and the muscles (musculotropic). Among the neurotropic substances there are the so-called Belladonna alkaloids or relatives. The best-known representative of this group is atropine, the name of which is derived from the black belladonna (Atropa belladonna).
Atropine is mainly used today for induction of anesthesia, in emergency medicine and ophthalmology, rarely for gastrointestinal cramps or colic of the biliary and urinary tract. In the last two areas of application, the substance butylscopolamine has increasingly replaced atropine.
The alkaloid atropine is also used as an antidote for poisoning with certain pesticides and is stored by the military against poisoning with nerve agents. The active ingredients glycopyrronium bromide, ipratropium bromide and tiotropium bromide help with asthmatic complaints. The neurotropic-musculotropic anticholinergics include, for example, oxybutynin and propiverine for treatments of the bladder or denaverine in gastroenterology and urology.
You can find your medication here
➔ Medicines for bladder and urinary tract healthRisks & side effects
The side effects of the Anticholinergics are numerous. Often fatigue, nausea, dizziness, poor concentration, circulatory disorders, constipation, visual disturbances, dry mouth and skin, urinary retention or intestinal weakness occur, with dry mouth being the most common side effect of all anticholinergic agents.
The influence on the nervous system can lead to states of confusion, memory disorders and restlessness. Elderly patients in particular suffer from increased memory impairments during treatment with anticholinergics. People who already have dementia can experience a deterioration in their cognitive performance due to the administration of anticholinergic medication.
Anticholinergics must not be taken in certain diseases or the dosage must be changed by the doctor. These include, for example, narrow-angle glaucoma, bladder emptying disorders, accelerated heartbeat (tachycardia), acute pulmonary edema or constrictions in the gastrointestinal tract. Due to the significant side effects of anticholinergics, a doctor should be discussed carefully and the cost-benefit factor weighed.

.jpg)











.jpg)







.jpg)