The Aortic arch syndrome is a stenosis of one or more arteries of the aortic arch. Congenital malformations of the bloodstream, autoimmune diseases and vascular diseases such as arteriosclerosis are possible causes. Treatment depends on the cause and usually involves vascular surgery.
What is aortic arch syndrome?

© lom123 - stock.adobe.com
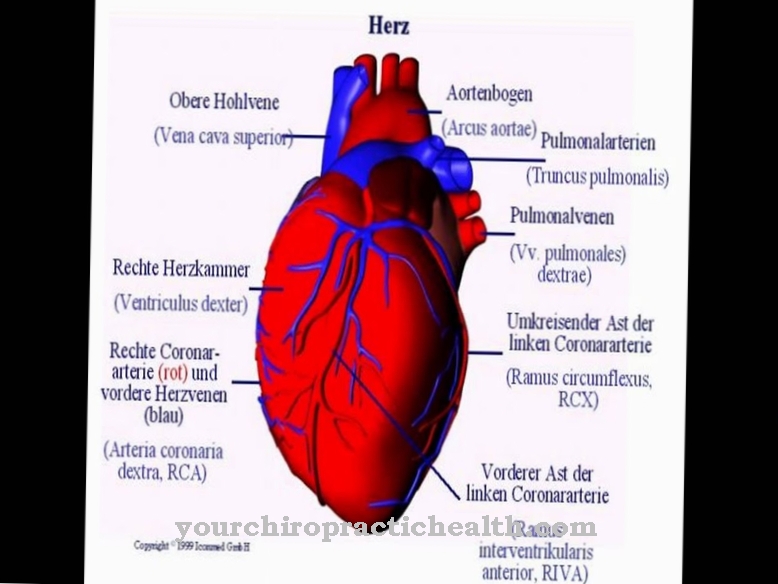
In aortic arch syndrome, one or more arteries that branch off from the aortic arch are narrowed. The disease is also called Mangold-Roth disease, Pulseless Disease or Obliteration syndrome designated. The aortic arch is in the immediate vicinity of the heart and is a section of the main artery that has several branches. In the case of aortic arch syndrome, the main artery can therefore also be involved.
In some cases, all branches of the aortic arch including the aorta itself are affected by stenoses, i.e. constrictions. The constriction can correspond to an existing occlusion or a partially existing occlusion. This phenomenon has an impact on blood pressure and the cardiovascular system, as well as on the perceptual structures and the brain. Aortic arch syndrome can be congenital. Acquired forms also occur and usually result from a vascular disease.
causes
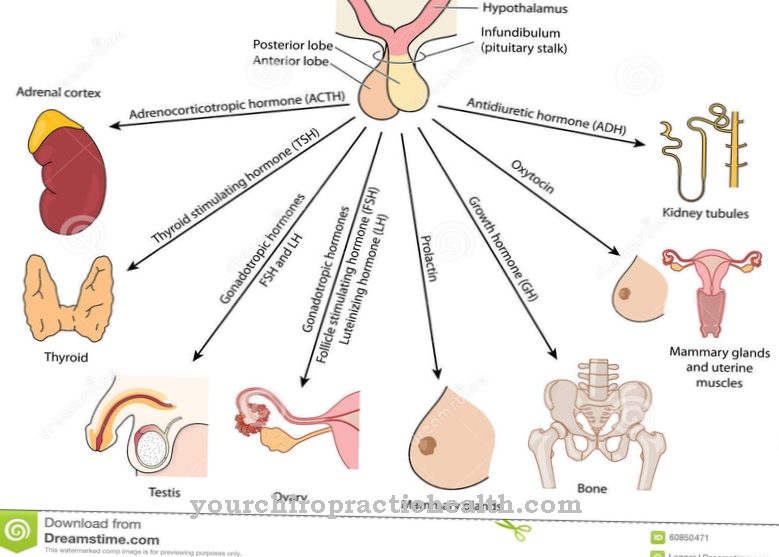
The congenital forms of the aortic arch syndrome are malformations of the vessels, as they occur in the context of various hereditary diseases. Congenital aortic arch syndromes are less common than the acquired form. Various vascular diseases can be the cause of the obliteration syndrome. The most common cause of the syndrome is Takayasu's arteritis or arteriosclerosis.
Takayasu's arteritis is an autoimmune disease in which the aorta and its main branches become inflamed. In arteriosclerosis, on the other hand, blood lipids, thrombi, connective tissue and calcium are deposited in the arteries and thus narrow the blood vessels. Endangiitis obliterans can also be a possible cause. This disease corresponds to systematic vasculitis of small and medium-sized arteries and veins. The above are just the most common diseases associated with aortic arch syndrome.
Symptoms, ailments & signs
Patients with obliteration syndrome show different symptoms, depending on which branches are affected by an occlusion and in the context of which disease the phenomenon occurs. For inflammation-related causes, those affected suffer from fever, for example. You are weak and losing weight. If the subclavian artery is affected by the occlusion, pain and paresthesia are the main symptoms.
A sensation of coldness and a reduced pulse frequency also arise in this context. There is arterial hypotension on the affected side. On the other hand, if the internal carotid artery is narrowed, neurological symptoms appear. In addition to dizziness and ringing in the ears, visual disturbances and other disorders of consciousness occur in particular.
Speech disorders and cognitive abnormalities may also occur. Paresthesias that primarily affect the face are just as conceivable. When the external carotid artery, the external carotid artery, is affected, the patient complains of pain in the jaw and temples.
Diagnosis & course
The doctor usually makes the diagnosis of aortic arch syndrome based on medical history and imaging tests such as sonography. Palpation of the arteries can also confirm his suspicion. However, imaging is absolutely necessary for the final diagnosis and to localize the occlusion. The course of the appearance is determined by how many and which arteries are affected by the occlusion. The cause and the severity of the occlusion also influence the course of the disease in individual cases.
Complications
Complications associated with aortic arch syndrome are highly dependent on the course of the causative factors and which of the arteries branching off the aortic arch are affected. These are always stenoses in one or more arteries that arise from the aortic arch. In some cases the aortic arch itself is also affected by a stenosis.
If the aortic arch syndrome remains untreated despite the underlying disease progressing, serious complications can arise. The way it is done depends on which of the branching arteries are affected by a narrowing and how severely. The arteries, which are responsible for supplying the head, neck and upper extremities, branch off from the aortic arch.
If one of the two carotid arteries is affected and parts of the head and brain are not optimally supplied with oxygen-rich blood and nutrients, sensory failures, a sensation of cold, a reduced pulse rate and low blood pressure can occur. Dizziness, tinnitus and visual disturbances often occur when the branching internal carotid, which supplies the front part of the brain to the forehead, is affected.
If the narrowing is caused by inflammatory processes and shows progression, it can lead to serious complications with a poor prognosis, unless treatment is given. Treatments, which can also include replacements for the affected artery sections, prevent such serious complications.
When should you go to the doctor?
The aortic arch syndrome comprises a broad and differentiated clinical picture. Depending on which of the arteries branching off the aortic arch have stenoses and which causative factors are involved. The prognosis for the further course of the disease also depends largely on the causative factors. For example, it is advisable to seek medical advice and appropriate therapy immediately if atherosclerosis is present or if the autoimmune disease Takayasu arteritis is detected.
In other cases, genetic predispositions play a role which have led to a slight to serious malformation of one or more arteries branching off the aortic arch. In these cases, only a slight progression of the disease is to be expected, so that if the parameters are otherwise normal, constant visits to a cardiologist or a vascular doctor (angiologist) are not necessary.
If, however, a fever develops, as well as pain, abnormal sensations in certain areas of the skin and concentration disorders, a visit to the family doctor or directly to the cardiologist or angiologist is urgently recommended. A visit to the specialist is also urgently required if dizziness, ringing in the ears, visual disturbances and sensations of cold occur. The above symptoms indicate that, for example, the right shoulder artery (arteria subclavia dextra) is affected by a serious stenosis because it can obviously no longer supply a part of the brain with sufficient oxygen and nutrients.
Doctors & therapists in your area
Treatment & Therapy
Treatment for aortic arch syndrome depends on the cause. If arteriosclerosis is the cause, reconstructive plastic surgery of the affected arteries is carried out, for example. This surgical intervention can be either angioplasty or thrombendarterectomy. During an angioplasty, the doctor dilates the affected bloodstream by inserting a catheter.
In thrombendarterectomy, the arteries are surgically exposed again. If occlusion is not significant, treatment can also be aimed at reducing atherosclerotic risk factors. The risk of thrombosis must also be reduced. Blood coagulation can be downregulated, for example. If, on the other hand, an autoimmune disease such as Takayasu's arteritis has been identified as the cause of the aortic arch syndrome, long-term treatment with immunosuppressants is carried out.
Severe constrictions can be removed by vascular surgical procedures. The surgical measures, however, require the patient to be in perfect condition. Above all, this means that there should be no severe inflammation in the organism at the time of the operation. Appropriate medication is given to treat inflammation. Sometimes a bypass anastomosis is suggested as part of aortic arch syndrome.
In this procedure, the doctor creates a bypass circuit. The blood no longer has to pass through the constricted blood vessels, but is diverted. The ends of different vessels are united in the anastomosis. This union can take place both end-to-end and sideways. In some cases, vascular prostheses are used in such anastomoses, which are incorporated into the vascular system.
Outlook & forecast
With today's medical options, aortic arch syndrome can usually be treated well. However, the prognosis is based on various factors. These include the severity of the damage, the time at which treatment was started and the age of the patient and their previous illnesses.
The more complex the blood vessels are affected, the more difficult it is to treat. Often it is not enough to achieve a permanent cure with just one procedure. If the narrowing of the arteries is noticed very late or not in time, the vessels can burst. There is a risk of serious illnesses that can lead to lifelong damage to the organism or have a fatal outcome.
The older a patient is, the weaker their age-related health is. If there are other diseases or impairments of the heart or blood vessels, the chances of recovery decrease. The emotional state of the patient is also important for a good prognosis. In the case of factors such as prolonged stress, trauma or a mental illness, the chances of recovery worsen.
In order to achieve lasting health improvements after a successful surgical procedure, lifestyle habits and physical stress often have to be adapted to the available options. If this is possible, a patient with an aortic arch syndrome can subsequently live symptom-free for a long time.
prevention
The arterioscleriotic aortic arch syndrome can be prevented by a consciously balanced diet, not consuming cigarettes and by taking sufficient exercise to regulate blood pressure. Little or nothing can be done about autoimmune diseases such as Takayasu arteritis or congenital malformations of the arteries. Thus, the aortic arch syndrome can only be influenced by individual lifestyle to a certain extent.
Aftercare
After successful treatment, aortic arch syndrome usually entails an adjustment in lifestyle. Patients must take appropriate measures on their own responsibility. This includes avoiding addictive substances such as nicotine and alcohol as well as losing weight. A balanced diet is just as important as adequate daily exercise. There is no immunity after illness.
The typical complaints can reappear. The syndrome can be congenital or acquired. The prognosis for old people is usually unfavorable. You need several mostly surgical interventions. Since the body does not regenerate as quickly with increasing age, there is a risk of permanent damage.
Doctors primarily use physical assessment and blood tests to diagnose. But imaging methods such as MRI, CT and Doppler sonography provide clarity about the progress of the aortic arch syndrome. The doctor will inform you about necessary appointments. Illness can lead to death.
Follow-up care aims to eliminate complications in advance. This often requires the help of the environment. Relatives can do a lot to take the stress of everyday life away from those affected. Since the aortic arch syndrome often occurs in combination with other diseases, an expansion of the treatment is necessary.
You can do that yourself
The behavior in everyday life and possible self-help measures depend on which of the arteries branching off the aortic arch are affected, how much the cross-section of the affected arteries is narrowed and what causes of the occurrence of the disease have been identified.
If, for example, the right subclavian artery is affected, restrictions in the central nervous system are also to be expected because the right carotid artery arises from the right subclavian and takes over part of the blood supply to the CNS. If only minor symptoms occur and the cause is a congenital disorder, no special behavior is required after clarification, apart from measures to inhibit blood clotting. This is to prevent the formation of a blood clot at the narrowed point of the artery.
One of the most important causes of acquired aortic arch syndrome is arteriosclerosis of one of the branching arteries. At the affected area, the cross-section of the artery narrows due to plaques being deposited in the middle wall (media). Plaques can form, for example, from insufficiently removed cholesterol fractions.
Here, too, anticoagulant measures are important to prevent a stroke or heart attack so that no thrombus can form, which can then be carried via the vascular system into the CNS or into the coronary arteries.
Basically, in these cases, a diet that contains as many natural food components as possible serves as a prevention against further arteriosclerosis and against progression of the existing arteriosclerosis.

.jpg)



.jpg)
.jpg)



.jpg)








.jpg)