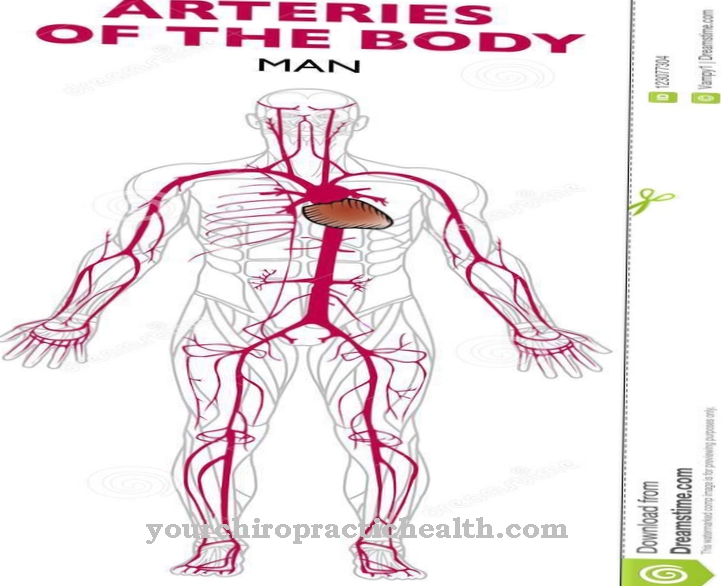
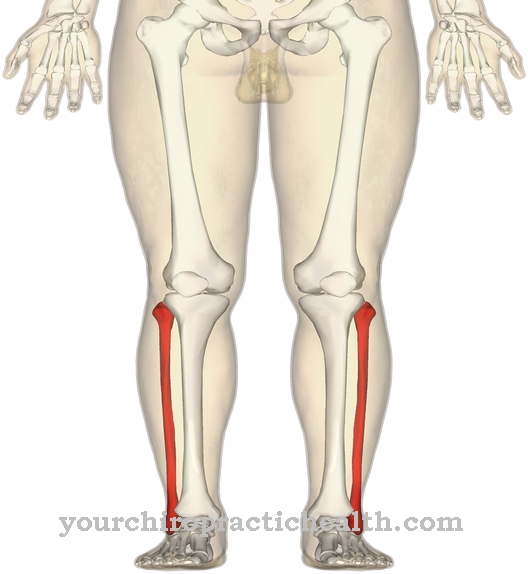
The Ulnar artery and the radial artery are the two main arteries of the forearm. They both arise from the bifurcation of the brachial artery in the crook of the arm. The ulnar artery runs along the ulnar to the wrist and reaches the hand via the carpal tunnel, where it supplies the three “ulnar” fingers and the ulnar part of the index finger with oxygenated blood.
What is the ulnar artery?
In the crook of the elbow, the brachial artery (upper arm artery) branches out in a bifurcation into the two forearm arteries, the arteria ulnaris (ulnar artery) and the arteria radialis (radial artery). The ulnar artery, which runs along the ulna through the carpal tunnel in the wrist and into the hand, supplies certain forearm areas, the ulnar fingers and part of the index finger with oxygen-rich blood.
On its way from the crook of the elbow to the ulnar fingers, a total of five main branches branch off from the artery, which supply certain areas of the forearm. At the wrist, a branch of the ulnar artery forms anastomotic connections with a branch of the radial artery. This creates a back-up system between the ulnar and the radial artery. If there is a bottleneck in one of the two arteries or the flow is completely blocked, the unblocked artery can take over the blood supply to a certain extent and serve as a kind of backup.
Anatomy & structure
The bifurcation of the brachial artery in the crook of the arm gives rise to two further forearm arteries, the ulnar artery and the radial artery. In its course along the ulna and in the area of the wrist through the carpal tunnel, a total of five main branches branch off in order to supply the corresponding areas with oxygenated blood.
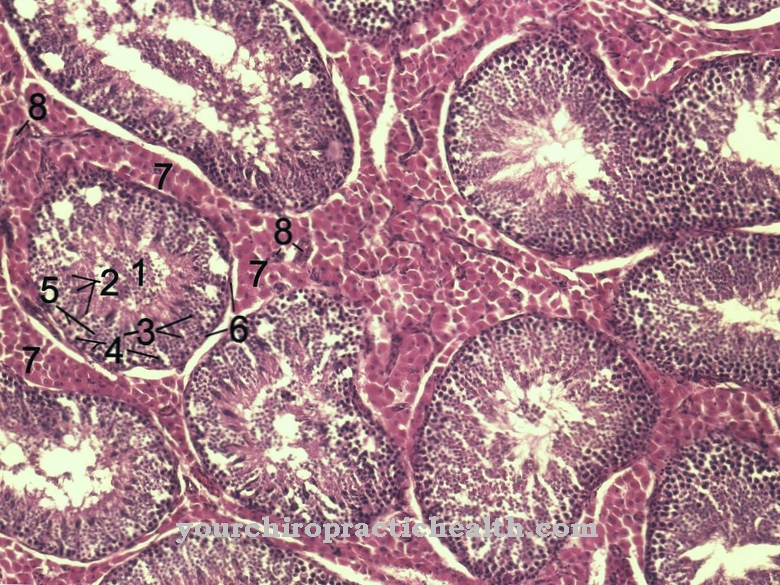
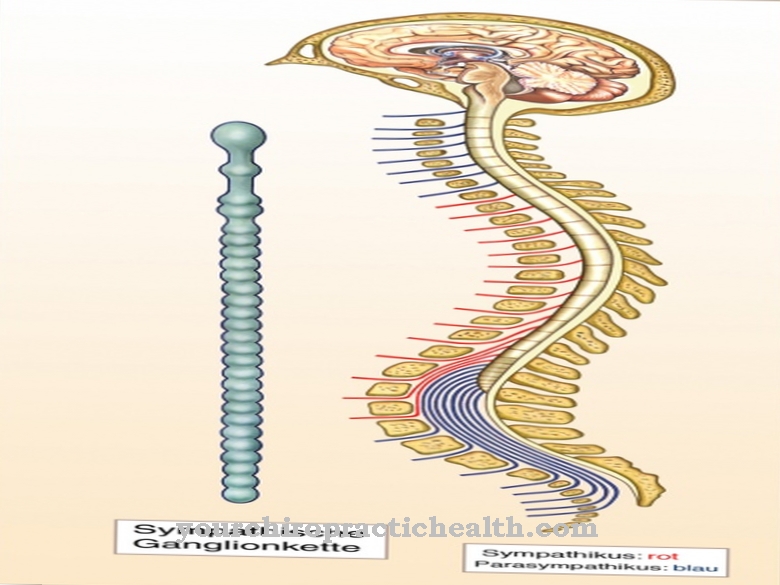
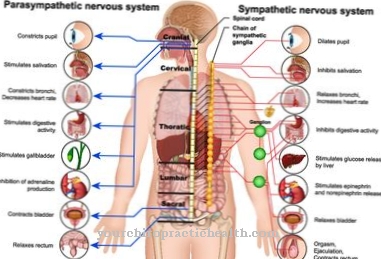
In the area of the wrist, the elbow artery forms the main supply network for the superficial palmar arch (arcus palmaris superficialis). The ulnar artery is a type of muscular artery that actively influences blood pressure regulation. In the middle of a total of three vessel walls, the tunica media, there are smooth muscle fibers as well as elastic and collagen fibers. The muscle fibers surround the media in a ring shape and sometimes obliquely ring-shaped, similar to the turns of a stretched helical spring. The smooth muscles of the ulnar artery are autonomously controlled by the sympathetic and parasympathetic nervous systems.
Stress hormones and other neurotransmitters cause the smooth muscle fibers to contract, resulting in a lumen reduction or vasoconstriction of the arteries in stressful situations and during intense physical activity. This leads to an increase in blood pressure. The parasympathetic nervous system can relieve tension by inhibiting the stress hormones.
In contrast to the muscular arteries, the large vessels close to the heart, such as the aorta, only have a passive influence on blood pressure because their media consists mainly of elastic fibers. The elastic fibers cause a strong increase in volume during the systolic tension phase of the heart chambers, so that the blood pressure peaks are smoothed and the necessary (diastolic) residual pressure is maintained in the subsequent relaxation phase, because the elastic walls of the large vessels contract again.
Function & tasks
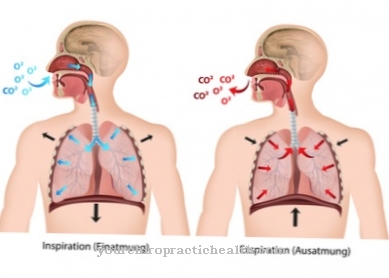
The primary task of the ulnar artery is to supply certain tissues of the elbow, forearm and hand with oxygen-rich blood. The oxygen-rich blood comes from the pulmonary circulation and reaches the main body artery (aorta) via the left atrium and chamber. The humerus artery branches off from the aorta and branches off into the ulnar and radial arteries.
The arterial side of the capillary system is supplied via arteries that branch off from the ulnar artery and are themselves usually subject to further branches. In addition to its primary supply function, the ulnar artery, together with other arteries of the muscular type, also takes part in the active control of blood pressure. Arteries, the vascular walls of which are largely made up of smooth muscle fibers, react in a contractile manner to certain messenger substances and stress hormones, so that the lumen of the vessels also narrows and causes blood pressure to rise.
The opposite effect occurs when the messenger substances and control hormones are collected again by the parasympathetic nervous system. Influencing and controlling the blood pressure are largely vegetative, i.e. unconscious. Participation in the control of blood pressure requires healthy, elastic vessel walls and an intact sympathetic and parasympathetic hormone control.
You can find your medication here
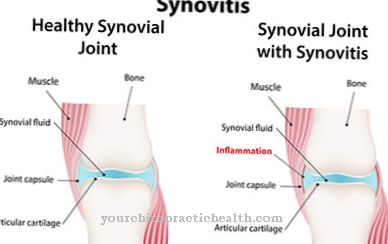
➔ Medicines for joint painDiseases
There are no known diseases or complaints that exclusively affect the ulnar artery. However, like all other arteries of the muscular type, the ulnar artery can be affected by functional disorders. In principle, local narrowing of the lumen of the artery, so-called stenoses, can occur.
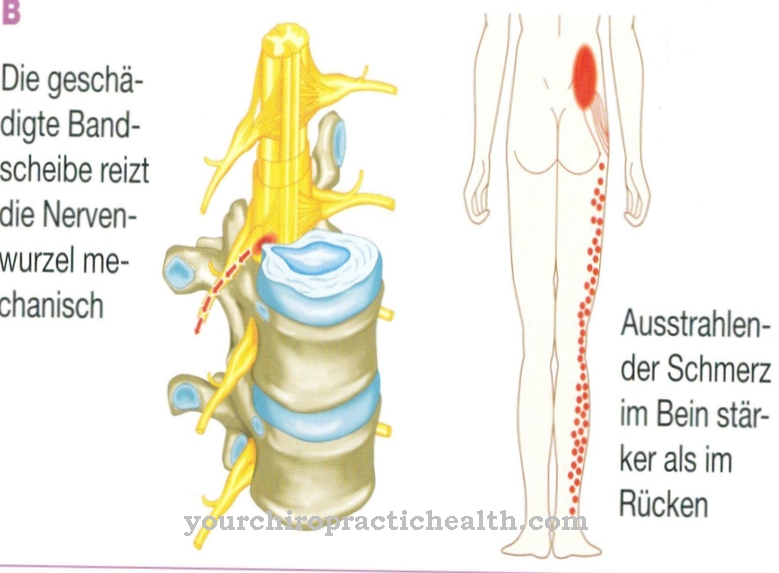
Depending on the severity, they lead to an insufficient supply of the downstream and branching arteries and thus to an undersupply of defined tissue parts. The most common reason for the formation of a stenosis is deposits, so-called plaques, in the vessel wall. The plaques can expand into the lumen and cause stenosis or even complete occlusion. In other cases, inflammatory reactions of the immune system can also lead to an accumulation of erythrocytes, which develop into a thrombus and block the artery in the form of thrombosis.
If such a thrombus develops elsewhere in the body - for example in the heart - it can be carried away with the bloodstream and accidentally become lodged in an artery whose cross-section is well below that of the thrombus. In this case there is an embolism. The effects of vascular occlusion caused by thrombosis or embolism are very similar. Only in extremely rare cases does the ulnar artery form an aneurysm, a bulging of the artery, which usually results from an injury to the artery. The lesion then forms the entrance portal for blood to flow between the inner and middle vessel wall.