Necrotic degradation processes of the human bone substance that cannot be traced back to an infection but to a vascular infarction are called aseptic bone necrosis designated. Depending on the location and type of aseptic bone necrosis, both sexes can be affected differently.
What is aseptic bone necrosis?

© joshya - stock.adobe.com
The term aseptic bone necrosis covers necrotizing diseases of the bone system which, in the absence of infection (aseptic), can be attributed to insufficient blood flow (ischemia) in the affected bone areas.
The closure of the supplying vessel (vascular infarction) causes the affected bone to be insufficiently supplied with oxygen, nutrients and minerals, which leads to a gradual breakdown and even to a possible functional failure of the bone area.
Aseptic bone necrosis can in principle affect all bones of the human skeletal system on one or both sides. Characteristically, aseptic bone necrosis manifests itself in the form of sudden or gradually increasing pain in the area of the necrotizing bone segment, which intensifies under stress and can radiate into neighboring skeletal sections.
In addition, movement restrictions of the affected area, especially in the later course of the disease, are possible with aseptic bone necrosis.
causes
Aseptic bone necrosis can usually be traced back to an occlusion of the blood vessel supplying the necrotic bone area. The exact etiology for this occlusion has not yet been clearly established.
In this context, constitutional factors, recurrent or iterative (repetitive) microtraumas and locally restricted circulatory disorders are discussed.
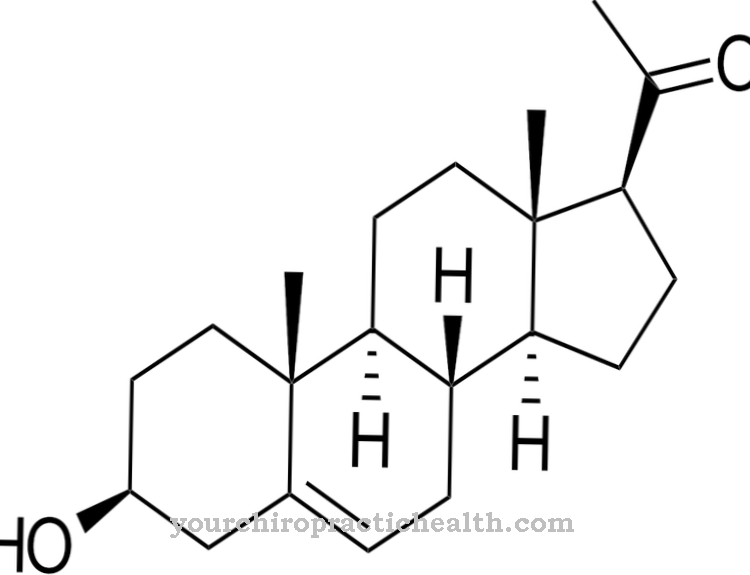
In addition, therapies with high-dose and systemically applied immunosuppressants (including sirolimus, glucocorticoids) or bisphosphonates (only for aseptic bone necrosis with involvement of the lower jaw), radiation and chemotherapeutic therapies (especially for lymphomas, leukemia), high pressure or activities in compressed air apply (Diving or compressed air environments such as in mining or tunneling), chronic nicotine and / or alcohol abuse, sickle cell anemia, Gaucher disease, HbSC disease, endocrine disorders, hyperlipidemia, metabolic disorders (diabetes mellitus), vascular and blood clotting disorders and the systemic form of lupus Erythematosus (SLE) as identified risk factors for aseptic bone necrosis, although the exact causal relationship is not known in every case.
You can find your medication here
➔ Medicines for painSymptoms, ailments & signs
Aseptic bone necrosis shows a creeping course of the disease, which means that symptoms are initially almost unnoticed, but then manifest more and more. The damage and degradation of the bone and often of the surrounding tissue cause discomfort in the directly affected area. The patient perceives an increasing pain that is mostly described as dull and persistent.
However, stabbing pain can also occur when the affected region is stressed. If the surrounding tissue is affected, it feels numb and can be painful. Damaged muscles lose their strength and resistance. The entire affected area feels numb and can no longer be stressed.
In the advanced stages of the disease there are usually fractures in the bones. These are extremely painful and usually occur suddenly under stress. The bone material loses its stability. Debris and spiral breaks are also very often diagnosed. In contrast to healthy bone, which usually breaks as a result of an event, the bone affected by bone necrosis is inherently unstable and breaks into many parts or fibers.
Bone necrosis cannot be reliably diagnosed by the patient himself, but is usually diagnosed during a medical examination or when a fracture has already occurred. If left untreated, it can lead to blood poisoning and death.
Diagnosis & course
In addition to a physical examination, functional tests of the affected bone and joint sections provide initial indications of aseptic bone necrosis. Diagnostic imaging methods such as x-rays or sonography enable statements to be made about possible pathological bone changes such as bone remodeling or destruction (especially in the later course of the disease).
In the context of magnetic resonance or computed tomography, early characteristic remodeling activities of the affected bone segments as well as the form and shape of the bone necrosis can be precisely determined. In terms of differential diagnosis, aseptic bone necrosis must be differentiated from septic necrosis, tumors and neoplasms of the bone and skeletal system and from bone cysts, osteomyelitis (inflammation of the bone marrow) or osteitis (inflammation of the bone).
The course and prognosis of aseptic bone necrosis depend on the severity and extent of the vascular infarction as well as the resulting damage to the affected joint or bone segment and the time of diagnosis or the start of therapy. In some cases, spontaneous healing of aseptic bone necrosis can be observed.
When should you go to the doctor?
In the event of sudden bone pain and restricted mobility, a doctor must be consulted immediately. As part of the medical diagnosis, it can then be determined whether aseptic bone necrosis is present.
If there is another disease of the bones or the musculoskeletal system, the doctor will refer the person concerned to the appropriate specialist. If aseptic bone necrosis is actually present, surgical measures must usually be initiated immediately.
People who suffer from sickle cell anemia, Gaucher's disease, metabolic disorders, vascular and blood clotting disorders or HbSC disease are particularly at risk for bone necrosis. Patients undergoing chemotherapy or radiation therapy are also more likely to develop aseptic bone necrosis. These risk groups should consult a doctor if they have unusual symptoms and have the cause clarified.
As part of the surgical treatment, the patient often receives an artificial hip replacement or a transplant with bone chips. Should any complaints arise during follow-up care, the responsible doctor must be informed immediately. There may be an inflammation or the body is rejecting the hip replacement. In any case, with aseptic bone necrosis, it is necessary to regularly consult with the doctor to avoid complications.
Doctors & therapists in your area
Complications
Aseptic bone necrosis is the general term used to describe the breakdown of one or more bones in the body. The symptom is not caused by the infection, but is caused by a vascular infarction. This no longer supplies the bone structure and the surrounding tissue with sufficient blood. As a result, the bone structure is destroyed.
Aseptic bone necrosis affects men and women equally. However, there are risk groups. These include patients with metabolic diseases, sickle cell anemia, divers, mountain farmers and alcoholics as well as taking immunosuppressive medication or undergoing radiation or chemotherapy. If the first signs of bone pain, which appear at rest as well as during exercise, are ignored, the symptom worsens.
The consequences of complications are restricted mobility, chronic persistent pain, rapid muscle breakdown in the affected bone, and functional failure of the arm or leg if the shoulder or hip are affected. In some cases, the affected area can be so painful that it also affects adjacent skeletal sections. The symptom is identified using imaging techniques. Since every ischemia of the bone is different, the therapeutic measures vary.
In general, aseptic bone necrosis can be treated successfully if detected early. In the case of particularly acute infestation, medication as well as radiation or chemotherapy are used. If bones or joints are completely destroyed, surgical procedures for an artificial replacement are necessary. The latter methods can cause tolerability complications for those affected.
Treatment & Therapy
In the case of aseptic bone necrosis, the therapeutic measures strongly correlate with the stage and extent of the disease and the general health of the person specifically affected.
For mild forms, the treatment aims to mechanically relieve the necrotic bone segment using forearm supports or orthotics, immobilization and physiotherapy with possible traction treatment. At the beginning of the disease, hyperbaric oxygenation (oxygen therapy) can be used as an accompanying or monotherapy, which has been shown to be particularly effective in painful bone marrow edema.
In the case of more pronounced forms of aseptic bone necrosis, surgical measures such as femoral head relief drilling (Pridie drilling), medullary canal decompression, adjustment osteotomies such as varization osteotomy for Perthes disease (femoral head necrosis) and transplants with bone chips are usually indicated. For example, as part of the Pridie drilling, the defective section of cartilage is drilled in order to enable blood vessel sprouting and to stimulate tissue regeneration accordingly.
A medullary canal decompression or core decompression (in the case of femoral or femoral head necrosis) is aimed at reducing the intraosseous (within the bone) pressure and slowing down the progress of the necrotizing processes.
In a punch cylinder reversal surgery, the necrotic areas are also removed and the body's own cancellous bone (spongy bone trabecular system) is inserted, while an intertrochanteric osteotomy rotates the necrotic focus out of the main stress zone, minimizes intraosseous pressure and stimulates vascularization (formation of small blood vessels).
If advanced bone destruction can be determined, endoprosthetics (artificial joint replacement) are usually indicated for the treatment of aseptic bone necrosis.
Outlook & forecast
The prognosis of aseptic bone necrosis depends on the existing bone vascular infarction. Its characteristics and influence on the supply of bones and joints are decisive for the prospect of healing.
Without medical care, the patient will experience pain and restricted mobility. Since there is no self-healing of the organism, the symptoms either remain suddenly or increase in intensity. A healing prospect is to be classified as extremely unlikely in this way.
With medical care of the vessels, the probability of a positive prognosis increases significantly. If there are other previous illnesses, the chances of recovery decrease again. In patients without additional illnesses and with a stable immune system, recovery takes place within a few weeks or months.
Complete freedom from symptoms is possible, but not always given. Corrections are made in a surgical procedure. In severe cases, the damaged joints are transplanted or replaced. The healing path is delayed because the organism has to come to terms with the new circumstances and the patient learns a new body awareness.
Following the inpatient stay, rehabilitation therapy is used to provide targeted training and exercises. In these, the movement sequences are optimized and adapted to the changed possibilities.
You can find your medication here
➔ Medicines for painprevention
Since the exact causes of aseptic bone necrosis have not yet been clearly clarified, the disease cannot be prevented. However, chronic alcohol abuse, for example, which is considered a possible risk factor, should be treated accordingly. In addition, the risk of aseptic bone necrosis (osteoradionecrosis) due to radiation therapy can be reduced by the prophylactic administration of anti-inflammatory drugs.
Aftercare
Patients must regularly consult an orthopedic surgeon as part of their follow-up care. The doctor will carry out various routine examinations such as an ultrasound examination and, if necessary, have further discussions that should allow an assessment of the condition. These regular follow-up checks will determine whether the necrosis has receded or whether it has spread.
On the basis of this, further measures are then initiated through which the healing process is further optimized. Aseptic bone necrosis progresses progressively and therefore requires long-term follow-up care. Patients must first see the doctor monthly or every two weeks. If the course is positive, the intervals can be extended.
However, patients must see screening at least every four to six months, regardless of the course of previous aseptic bone necrosis. If complications are found, further examinations are always required. Follow-up care also includes a mobility check.
A physiotherapist will examine the patient and, if necessary, give tips for further treatment. The detailed follow-up measures required always depend on the individual course of the disease. Patients should contact their doctor during treatment and discuss the next steps with them.
You can do that yourself
In addition to medical therapy, patients with aseptic bone necrosis can themselves contribute to improving the disease and wellbeing. Adhering to rest periods and avoiding stress are beneficial for therapy. Mechanical relief through orthoses or crutches can be useful, as well as not using cortisone medication. The attending physician puts together the ideal medication.
Physiotherapy and massages help maintain and improve joint mobility. In physiotherapy, exercises and acupressure moves can be learned, which can then be used at home. It is advisable to support medical therapy with moderate exercise. The blood flow should be gently increased here. Yoga and moderate exercise such as cycling on the stationary bike, swimming, or walking are good supplements. The movement has a positive effect on the mood as well as on the metabolism and circulation.
A balanced diet is also part of the therapy for aseptic bone necrosis. The focus here is on controlling or reducing blood lipid levels and weight. The Mediterranean diet with a high proportion of omega-3 fatty acids, little red meat and a lot of fish is ideal. Fresh vegetables and fruits should not be missing. Avoiding alcohol and nicotine, on the other hand, promotes therapeutic success. Likewise, good introspection and early consultation with a doctor if symptoms appear or worsen.



.jpg)











.jpg)





.jpg)