The asphyxiating throax dysplasia is a short-rib polydactyly syndrome. The narrow thorax of the patient usually causes a thoracic respiratory insufficiency. If those affected survive the first two years, the risk of death in the future is greatly reduced.
What is asphyxiating thoracic dyplasia?

© eveleen007 - stock.adobe.com
Asphyxiating thoracic dysplasia is and is a skeletal dysplasia from the group of short-rib polydactyly syndromes Jeune Syndrome called. This name goes back to the pediatrician M. Jeune, who first described the phenomenon in 1954. The congenital malformation of the chest is one of the ciliopathies. One to five people affected per 500,000 newborns are given as the ratio for the incidence.
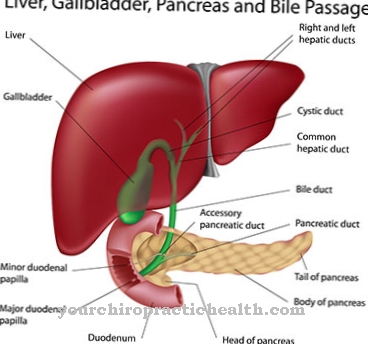
The disease is hereditary and is usually characterized by extremely short ribs and an extremely narrow thorax. There may be multiple organ involvement, such as those of the liver and pancreas. Although the disease is usually associated with an unfavorable course, there are exceptions to this rule. After the age of two, the worst is over.
causes
Skeletal dysplasia Jeune syndrome is inherited in an autosomal recessive manner. This means that the affected gene is on an autosome. A dominant allele always prevails over a recessive allele in genetics. For the disease to actually break out on a recessive autosome, both partners must have at least one recessive allele as a disease carrier. Jeune syndrome can occur due to mutations in different genes.
Not all genes are known so far. One example is the IFT80 gene (3q25.33). The same applies to the DYNC2H1 gene (11q22.3) and the WDR19 gene (4p14). A mutation of the TTC21B (2q24.3) gene is now recognized as a possible cause of Jeune syndrome. Each of the genes mentioned codes for one flagella transport protein. For this reason, the disease is also counted among the so-called cilliopathies.
You can find your medication here
➔ Medication for shortness of breath and lung problemsSymptoms, ailments & signs
People with Jeune syndrome have a long and narrow thorax.The horizontal roof of her pool is also striking. They usually suffer from shortness of breath from birth, as their lungs hardly have any space in the dysplastic chest. We are talking about a thoracic respiratory failure. This means that the shortness of breath is caused by the lack of space in the chest. Often the patient's lungs are even underdeveloped because of the minimal space available.
As with all other diseases from the group of short-rib polydactyly syndromes, many sufferers have polydactyly, i.e., multiple fingers. Other skeletal abnormalities can occur. Short extremities and short stature are common phenomena. Renal insufficiency due to nephronophthisis often occurs later. In addition, retinopathy, i.e. retinal disease, can occur. Jaundice and fibrocytic changes in the liver and pancreas are also common as part of the disease.
Diagnosis & course
While the fetus is still in the uterus, the diagnosis of Jeune syndrome can be made through careful ultrasound examinations. For the most common form of the disease, there is also the possibility of a prenatal diagnosis in terms of molecular genetics. If this option is not used, the diagnosis is made immediately after birth through visual diagnosis and radiological findings.
Jeune's syndrome is fatal in many cases, but the prognosis is more favorable the less the internal organs are affected by functional disorders. Depending on the type of ossification of all cartilage systems, there are two different forms of the disease, which are also known as type I and type II. Ultimately, the impairment of the lungs determines how promising the treatment of asphyxiating throaxic dysplasia is. After the age of two, the risk of infections decreases significantly.
Complications
Asphyxiating thoracic dysplasia is the rare malposition of a chromosome. From birth, those affected have a narrow, long-acting thorax with short ribs. Due to the physical limitation of the chest, the lungs are severely underdeveloped, which leads to acute circulatory weakness and respiratory depression.
Those affected are short and have short extremities and long bones. Skeletal dysplasias usually have numerous complications and do not progress positively as the patient ages. Especially in newborns there is difficulty breathing because the thorax is too narrow. Renal insufficiency can develop at a young age. There is also a risk of fibrosis of the pancreas and liver.
The lungs that are too tight are susceptible to infection and can cause respiratory paralysis and spontaneous respiratory failure. There is a risk of cardiovascular failure. As the child grows up, complications increase and diabetes with accompanying poor eyesight can occur. The symptom can already be detected in the womb during screening.
The degree of severity and the method of treatment are subject to the case-dependency. As a first therapeutic method, normalization of the ventilation parameters is being considered, whereby the rib thorax is surgically stretched. The surgical risk outweighs the child's chances of survival. Patients with asphyxiating thoracic dysplasia require medical supervision for the rest of their lives with regard to organ function and physiotherapeutic measures to keep the impaired musculoskeletal system mobile.
When should you go to the doctor?
Asphyxiating thoracic dysplasia can usually be suspected immediately after the birth. The disease manifests itself through clear physical characteristics (including short, horizontally running ribs, unshortened tubular bones) that are noticed by the responsible doctor, the obstetrician or the parents themselves. The diagnosis is then secured with the help of an X-ray image.
Which subsequent treatment steps are possible depends, among other things, on the severity of the dysplasia. In less severe cases, it is sufficient to treat the infections that occur and to regularly check the kidney and liver function. Occasionally, novel treatment options such as VEPTR (Vertical Expandable Prosthetic Titanium Ribs), which require a longer hospital stay, have to be used.
The doctor responsible will suggest the appropriate treatment and, in consultation with the parents of the child concerned, make appointments for the treatment. Even with successful treatment, the person concerned must have regular examinations carried out. In the event of a sudden deterioration in health, an asphyxiating chest dysplasia should be taken to hospital immediately.
Doctors & therapists in your area
Treatment & Therapy
When treating asphyxiating throat dysplasia, the doctor must first try to keep the upper airways free of infection. Depending on which additional symptoms make up the disease in the individual case, he must also take action against kidney failure and against fibrosis of the liver and pancreas. If the patient is suitable for this procedure in individual cases, the VEPTR procedure may be used.
This surgical technique aims to permanently expand the thorax. A vertically expandable rib prosthesis made of titanium is inserted into the patient to pry open the chest. The affected person is placed under general anesthesia with the titanium rib. The titanium rib has a curved shape and several holes for fixation in the required length. The titanium rod is either wedged between two ribs or attached between a rib and the pelvis. The spine is straightened up indirectly. The thorax increases in volume and the lungs have more space.
Several surgeries may be required to expand the chest to the desired volume. Patients are only selected for this procedure if the operation can be expected to have promising results in their individual case. As long as there are infections of the respiratory tract, an operation like this must not take place anyway. Combating respiratory infections and stabilizing the patient before the operation is therefore imperative.
Outlook & forecast
The prognosis for asphyxiating thoracic dyplasia is very poor. Many sick people die within the first months of life or years after birth. Given the current scientific and medical possibilities, the disease is considered incurable. There is a genetic disposition that cannot be corrected.
For legal reasons, research and treatments on human genetics are restricted and prohibited. As a result, there are insufficient treatments available to alter the skeletal system in such a way that it can cure or at least relieve symptoms.
The internal organs do not have the space in the chest that they need to be able to carry out their activities. This leads to functional disorders and, in particular, severe shortness of breath. There is also a high risk of death with artificial respiration. With the increasing growth and development process of the body, the space for the organs, vessels and surrounding tissue narrows immensely. The process cannot be prevented.
If children survive the growth process, their life expectancy is still not very high. The death rate is exorbitantly high in adults with asphyxiating thoracic dyplasia. A significantly reduced life expectancy leads to poor prognosis prospects. This condition is all about relieving pain and minimizing patient suffering.
You can find your medication here
➔ Medication for shortness of breath and lung problemsprevention
Since asphyxiating throax dysplasia corresponds to a gene mutation, the disease cannot be prevented. For parents who have already given birth to a child with asphyxiating throaxial dysplasia, the probability of a second child with the disease is 25 percent.
Aftercare
In the case of this disease, the person affected usually has no or very few measures and options for follow-up care available. First and foremost, a comprehensive diagnosis and subsequent treatment must be carried out in order to prevent further complications. Neither can self-healing occur, so treatment by a doctor must definitely be carried out.
The earlier the doctor is consulted about this disease, the better the further course of the disease is usually. A complete cure is not possible because it is a hereditary disease. If the person concerned wishes to have children, hereditary advice can be useful so that the syndrome is not passed on to the descendants.
With this disease, the person affected is usually dependent on the care and support of their own family. Loving and intensive conversations also have a positive effect on the course of the disease and can also prevent psychological upsets or depression. This disease may also reduce the patient's life expectancy.
You can do that yourself
Asphyxiating thoracic dyplasia, also known as Jeune syndrome, is a hereditary disease. Those affected have no way of treating the cause of the disorder.
Asphyxiating thoracic dyplasia is already evident in the fetus and can be detected by an ultrasound examination. If this disorder is suspected, additional methods of prenatal diagnosis are available. Jeune syndrome is associated with very serious health problems and is usually fatal. Medically indicated termination of pregnancy is therefore possible up to the 24th week of pregnancy.
Women who nevertheless decide to carry the pregnancy to term must expect the child to die within the first two years. This represents an enormous psychological burden for young parents. You should therefore seek advice and help from other affected persons at an early stage and do not be afraid to seek help from a psychologist.
Since the first two years of life are particularly critical for patients with Jeune syndrome, the families of affected children are confronted with constant visits to the doctor, hospital stays and home nursing during this time.
How this additional organizational burden can be integrated into everyday (professional) life should be clarified during pregnancy. Self-help groups and the health insurance companies provide information about financial and organizational support options.


.jpg)




















.jpg)



