Under a Pheochromocytoma an adrenal market tumor is understood. He is able to produce hormones.
What is a pheochromocytoma?

© SciePro - stock.adobe.com
At a Pheochromocytoma it is a tumor in the adrenal medulla. In most cases, the hormone-producing tumor is benign. The hormones produced are mostly adrenaline and noradrenaline. In 85 percent of all cases, the tumor is on the adrenal gland. While 85 percent of all pheochromocytomas are benign in nature, 15 percent develop a malignant course. 90 percent of the tumor is one-sided. With the remaining 10 percent it settles on both sides.
The paraganglioma is a rarely occurring form of pheochromocytoma. The tumor runs along the sympathetic trunk outside the adrenal glands. This is located in the stomach and chest region in the spine area. Pheochromocytoma rarely occurs. Two to eight cases of illness occur in around one million people. Adults are particularly affected by the disease, but children also sometimes suffer from the tumor.
causes
The cause of the development of a pheochromocytoma cannot always be found out. In medicine, there is talk of a sporadic pheochromocytoma. This type of tumor appears predominantly between the ages of 40 and 50 years. Some forms of pheochromocytoma are hereditary. They arise through mutations within the genome and mostly occur in younger people under 40 years of age. About 10 percent of these pheochromocytomas show up in families.
In some cases, pheochromocytoma is associated with other hereditary diseases. These include Von Hippel Lindau Syndrome, Multiple Endocrine Neoplasia Type 2 and Neurofibromatosis Type 1. A typical feature of pheochromocytoma is the increased production of stress hormones such as adrenaline and noradrenaline. The tumor can also produce dopamine, but this is less common.
Symptoms, ailments & signs
The increased release of adrenaline and noradrenaline leads to the symptoms of pheochromocytoma. However, the complaints vary from person to person. Some patients even show no symptoms at all, which means that the tumor is only discovered by chance. A typical symptom of pheochromocytoma is high blood pressure. This leads to an abrupt and seizure rise in blood pressure, which can even reach life-threatening proportions.
Doctors then speak of a hypertensive crisis or a blood pressure crisis. About 50 percent of all patients are affected by this symptom. Occasionally, blood pressure can also be chronically high, which is known as persistent hypertension. Around half of all adult patients and around 90 percent of all children suffer from it.
There are other symptoms of pheochromocytoma possible. These include weight loss, angina pectoris, headaches, sweats, racing heart, tremors, anxiety and paleness of the face. The high adrenaline level also causes blood sugar levels to rise. There is an increased risk of developing diabetes mellitus as the disease progresses.
Diagnosis & course of disease
The diagnosis of a pheochromocytoma is usually based on the typical symptoms. The occasional high blood pressure attacks, for which the usual medication treatments have no effect, are primarily considered suspicious. It is also important to measure the stress hormones adrenaline and noradrenaline. For a reliable measurement, either a urine sample, which is collected 24 hours, or an examination of the blood plasma within 30 minutes.
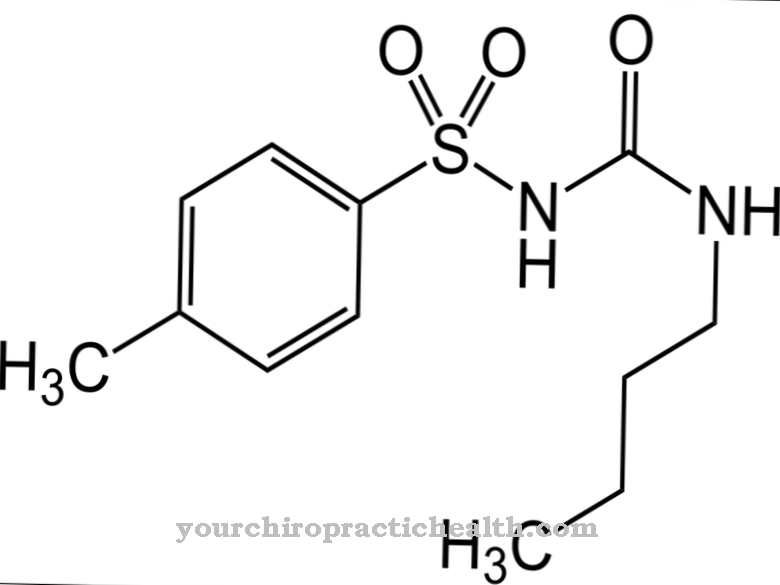
If there is an increased hormone content, a clonidine inhibition test is carried out. Clonidine is one of the active substances against high blood pressure. While clonidine inhibits the release of adrenaline in healthy people, the value remains high in the case of a pheochromocytoma. Imaging methods such as computed tomography (CT) or magnetic resonance imaging (MRI) are used to detect a pheochromocytoma.
A special MIBG scintigraphy is performed to localize a tumor that is located outside the adrenal gland. The course of the disease in a pheochromocytoma is different. In around 80 percent of all patients, blood pressure returns to normal after the tumor has been successfully removed. However, the remaining patients have high blood pressure because other causes also play a role. A pheochromocytoma recurs in around 15 percent of all those affected.
Complications
The symptoms of pheochromocytoma can be very different. For this reason, the complications and symptoms can usually not be universally predicted. In most cases, however, this disease leads to high blood pressure. Those affected can also suffer a heart attack, which in the worst case leads to death.
General malaise and hypertension can also occur and usually have a very negative effect on the patient's everyday life. Those affected often suffer from anxiety or sweating. A racing heart or severe headaches can also occur as a result of the illness. Furthermore, there is also paleness in the face and palpitations. If the pheochromocytoma is not treated, it can also lead to diabetes.
When treating pheochromocytoma, the tumor that is causing the symptoms is usually removed. It cannot be universally predicted whether this will lead to complications.Chemotherapy is also usually necessary. Pheochromocytoma may also reduce the person's life expectancy.
When should you go to the doctor?
Since a pheochromocytoma is a tumor, it must be treated by a doctor immediately. The earlier treatment and diagnosis occur, the higher the chances of a complete cure. Often the tumor itself is discovered only by chance, as it does not lead to any clear symptoms. After the diagnosis, however, it must be removed quickly. In many cases, the pheochromocytoma is manifested by high blood pressure. If the high blood pressure occurs without a particular reason and, above all, permanently, a doctor should be consulted. The blood pressure itself is often chronically elevated. The pheochromocytoma is also noticeable through a loss of weight, paleness of the face or through strong sweats. Consult a doctor if you have any of these symptoms.
As a rule, the first examination can be carried out by the family doctor. However, a more detailed examination and possibly treatment will require a specialist doctor. Whether the pheochromocytoma will lead to a reduced life expectancy for the patient cannot generally be predicted.
Therapy & Treatment
Surgical removal of the tumor is considered the best treatment for pheochromocytoma. Most patients undergo minimally invasive laparoscopy for this purpose. Only three smaller incisions need to be made on the abdominal wall. After inserting the surgical instruments, the surgeon finally removes the tumor. If the tumor is larger or difficult to remove, a more extensive laparotomy may be necessary.
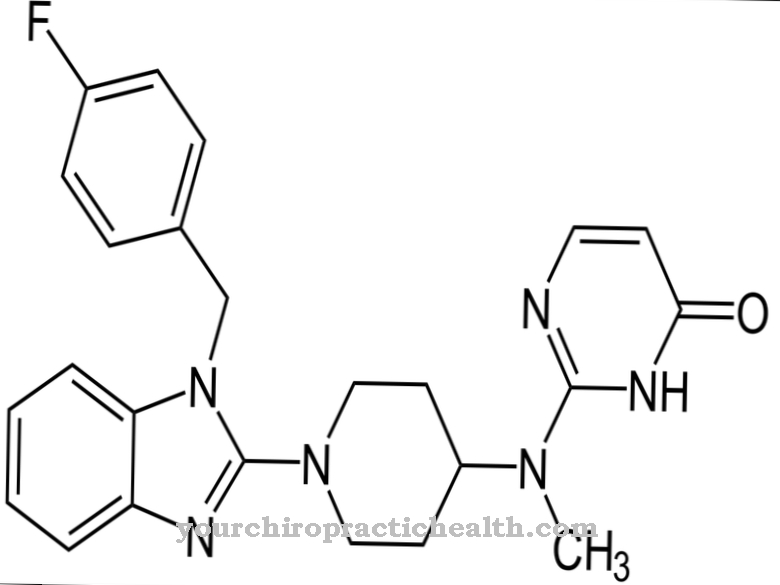
If both adrenal glands are affected by a pheochromocytoma, this results in a steroid hormone deficiency after an operation. To compensate for this, the missing hormones are replaced with drugs. Further treatment depends on whether the pheochromocytoma is benign or malignant. A malignant tumor can lead to the development of metastases (daughter tumors). Chemotherapy or radio-iodine therapy are conceivable as possible therapeutic measures.
Sometimes it is not possible to treat a pheochromocytoma surgically. In such cases symptomatic therapy takes place. This treats the complaints that occur due to the excessive production of stress hormones. For example, alpha blockers can reduce the adrenaline effect by blocking the docking points.
Outlook & forecast
The prognosis for a pheochromocytoma varies and depends on several factors. If it is possible to operate on the tumor at an early stage and if the patient does not suffer from additional diseases, the outlook is usually favorable. The symptoms often go away again. In around 50 to 80 percent of all affected people, blood pressure returns to normal after a surgical procedure, provided that it is a benign pheochromocytoma.
If the patient has been suffering from pheochromocytoma for a long time, there is a risk of secondary symptoms such as heart failure due to the increased blood pressure. Around 15 percent of all those affected have to expect that a pheochromocytoma will recur after treatment. The doctors then speak of a relapse. For this reason, the patient should have check-ups at regular intervals. They serve to detect a possible relapse in good time so that an effective treatment can be carried out.
If a benign phaeochromocytoma is surgically removed, essential hypertension still exists. This means that the blood pressure will continue to be high because other triggers are also present. If a benign pheochromocytoma is present, 95 percent of all patients will survive the next five years. If, however, it is a malignant tumor and metastases have already formed, the 5-year survival rate drops to around 44 percent.
prevention
Preventing a pheochromocytoma is not possible. However, genetic counseling can be useful for families with a predisposition.
Aftercare
With a pheochromocytoma, the affected person has only very limited measures and options for follow-up in most cases. Since this is a tumor on the kidneys, a doctor should be contacted very early so that there are no complications or other complaints in the further course. The earlier a doctor is consulted, the better the further course of the disease is, as a rule, since no spontaneous healing can occur.
Most of those affected are dependent on an operation. The affected person should definitely rest after such an operation and take care of his body. Exertion or stressful and physical activities should be avoided in order not to continue to burden the body. Most of those affected with pheochromocytoma also depend on the support of friends and family in everyday life.
It is not uncommon for psychological support to be also very important so that there are no psychological upsets or depression. Regular checks and examinations by a doctor are also very important in order to detect and remove further tumors at an early stage. In some cases, the pheochromocytoma reduces the life expectancy of those affected.
You can do that yourself
A pheochomocytoma is usually removed surgically. What measures the patient can take afterwards to recover quickly depends on the location of the tumor and other factors.
In principle, nothing should be eaten in the first few hours after the procedure. After a general anesthetic, you must also refrain from drinking. After one day, the patient is allowed to eat bland foods again. The doctor will make precise guidelines on nutrition and, if necessary, involve a nutritionist. To compensate for the loss of nutrients and fluids, you should eat and drink enough in the days and weeks after the pheochomocytoma operation. Food supplements and infusion solutions are also available. Alcohol should be avoided in the first few weeks as it has a negative effect on blood clotting.
In addition, physical protection always applies. The part of the body that has been operated on is particularly sensitive to pain and must not be exposed to strong vibrations. Instead, careful cooling is recommended. After the pheochomocytoma has been removed, additional symptoms may appear initially. These should have subsided after a few weeks at the latest. If the symptoms persist, it is best to inform the doctor.

.jpg)
.jpg)
.jpg)






.jpg)
.jpg)







.jpg)