When bacteria penetrate the bloodstream, there is one Bacteremia in front. Normally, a healthy immune system eliminates the bacteria before they can spread widely and reach vital organs through the blood. In patients with a poor immune system, however, bacteremia can result in severe sepsis.
What is bacteremia?

© Giovanni Cancemi - stock.adobe.com
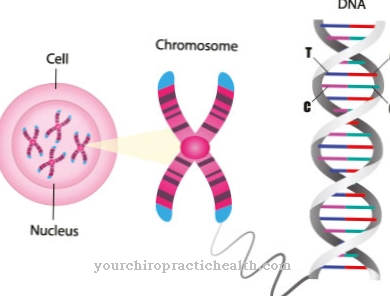
Bacteria are everywhere: in the air, on everyday objects and on your own skin. The immune system becomes active at the latest when bacteria are washed into the bloodstream. As a rule, the microorganisms are eliminated in the bloodstream. If this elimination by the immune system does not take place, bacteremia can develop.
Bacteria are part of the healthy human skin and mucous membrane flora. This is to be distinguished from bacteria, which are generally considered to be pathogens and which harm humans when colonizing them. The phenomenon of bacteremia occurs in the serum detection of bacteria. It can be temporary or chronically extended over a longer period of time. Viraemia, in which viruses spread in the blood, must be differentiated from bacteremia.
A related phenomenon is fungemia, or mycemia, in which fungi produce similar conditions. The human immune system takes over the fight against bacteria after they have been washed into the blood. A healthy immune system recognizes bacteria as foreign and attacks them, so that immunologically healthy people often only suffer from temporary bacteremia.
Chronic bacteremia occurs far more often in immunodeficient patients and can be caused in them by commensals, which as a rule do not harm a healthy person.
causes
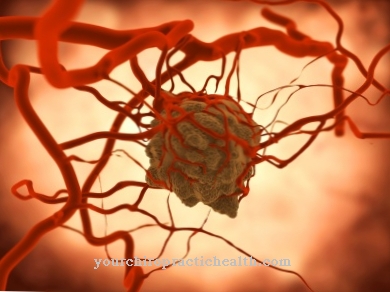
Sepsis in the sense of blood poisoning with systemic signs of inflammation of the entire organism can result. Septicopyemia often occurs, in which the pathogens spread further and further in the blood and thus reach vital organs, where they cause inflammation. The cause of bacteremia is the spread of bacteria into the blood.
Existing wounds form a gateway. In addition, bacteria can enter the bloodstream via bacterial abscesses as soon as fistula ducts form. Abscesses play an important role in everyday clinical practice. They are caused by inflammatory tissue melt-downs that are triggered by bacterial infections. The abscess cavity of the melted tissue is filled with pus from dead cells, neutrophils, and bacteria.
Untreated abscesses continue to spread along crevices. After the formation of a fistula, the abscess cavity empties into internal or external body surfaces.Bacteremia after invasive medical interventions were also widespread, especially in the past. The bacteria either reach the blood in the case of bacteremia, i.e. as a result of a bacterial infection elsewhere, in the course of diagnostic or therapeutic interventions, or are carried away from the skin into the blood through smaller wounds.
Symptoms, ailments & signs
Bacteremia is always present when cultural evidence of bacteria in the blood can be provided. Some patients show no symptoms of brief bacteraemia apart from exhaustion. Sepsis or septic shock do not necessarily have to occur. Sepsis corresponds to an infection with general signs of inflammation.
As soon as sepsis affects organs, it is referred to as severe blood poisoning. In the case of septic shock, the patient's circulation breaks down. In a healthy person, bacteremia is the temporary presence of bacteria in the bloodstream that often clears itself up when the immune system attacks.
An excessive multiplication of the bacteria or the settlement of the pathogens in organs usually does not arise from bacteremia for healthy people. As soon as they reach the blood, the healthy immune system recognizes them as foreign and combats them so that they cannot metastasize into organs. Bacteremia is usually only associated with sepsis if the person's immune system is excessively poor, for example in HIV patients or immunosuppressed people.
If the bacteria from an infectious source are constantly or periodically washed into the bloodstream, they multiply rapidly and thereby cause sepsis. Which other symptoms are present depends on the type of bacteria and the aggressiveness of the pathogen. For patients with poor immune systems, bacteremia can lead to a serious increase in the number of microorganisms. Different organs can be affected. A disease caused by bacteremia in predominantly immunodeficient patients is, for example, bacterial endocarditis.
Diagnosis & course
Bacteremia is diagnosed by serological evidence of bacteria in the blood. The diagnosed patient is further observed in order to be able to estimate the duration of the bacteremia and to identify any signs of sepsis promptly. The prognosis depends on the immunological constitution of the patient and the type of pathogen that has invaded.
Complications
In most cases, bacteremia can be treated relatively well. The treatment itself takes place with the help of antibiotics and in most cases leads to relatively quick success. It becomes problematic when the bacteria are multi-resistant. Extensive treatment and possibly a blood transfusion is necessary here.
If the bacteria cannot be removed from the body, all organs of the patient must be monitored. This can lead to serious infections and inflammations that can be life-threatening. Usually the patient has to be transferred to the intensive care unit in the hospital.
Without treatment, bacteremia need not necessarily lead to complications. In many cases, the body can fight back against the symptom and defeat the bacteria on its own. However, bacteremia makes the body more susceptible to various diseases. The immune system and the circulatory system are both weakened and can break down more easily.
This results in a general sluggish attitude towards life and fatigue. In the worst case, the spread of bacteremia can lead to death in a person if the symptom is not treated in a timely manner. Bacteremia is an increased risk, especially in older people, and should therefore always be treated by a doctor.
When should you go to the doctor?
If a wound becomes infected or other infections are noticed, the family doctor should be consulted. By examining the inflamed area and doing a blood test, the doctor can quickly determine whether bacteria have entered the blood and, if necessary, initiate treatment directly. If inflammation is left untreated, bacteremia will show up at the latest in increasing exhaustion. If this symptom is noticed, it is advisable to see a doctor immediately. Especially people with an immune deficiency (e.g. HIV patients or immunosuppressed people) should speak to a doctor if they have unusual symptoms.
Above all, serious infections and increasing cardiovascular complaints indicate the onset of sepsis. An external warning sign is a reddish stripe on the skin that leads from the inflammation towards the heart. In the event of fainting or cardiac arrhythmias, the emergency doctor must be called. In severe cases, first aid measures must be taken until the emergency services arrive. Since advanced bacteremia requires a longer stay in hospital, the relatives should also be informed.
Doctors & therapists in your area
Treatment & Therapy
In the case of bacteremia, the patient is immediately provided with a suitable drug that prevents the pathogen from multiplying. In most cases, at least one of the currently used antibiotics is working. Identifying the microorganisms is necessary in order to select an antibiotic for treatment. Most strains of bacteria are resistant to at least one of the medically used antibiotics.
The treatment of bacteremia is particularly difficult if the bacterium involved is multi-resistant. In such cases the conventional antibiotics usually do not work and the bacterium can hardly be stopped from multiplying. Multi-resistant bacteria have become known from various hospital infections.
In bacteraemia, especially for immunodeficient patients, they can cause life-threatening infections of various organs without them being medically controlled. If the bacterium and with it the cause of the infection cannot be eliminated, the medicine mainly focuses on damage control.
In this case, the focus is on maintaining all vital body functions. Patients are usually monitored in the intensive care unit, where life-sustaining measures such as resuscitation can be carried out more quickly.
Outlook & forecast
The prognostic outlook for bacteremia depends on the bacterial culture that has entered the organism. The germs that penetrate can usually be treated with medication. The multiplication of the pathogens is stopped and the bacteria die off within a few days. At the same time, health improves again until the patient has completely recovered after a few weeks.
Some patients suffer from intolerance to the drug. This creates a challenge in fighting the bacteria and can make the healing path much more difficult. Alternative drugs exist, but their active ingredients are less effective than antibiotics. Most types of bacteria die even without medical treatment.
After it has penetrated the organism, the immune system gradually builds up enough defenses and thus has the strength to remove them from the bloodstream. However, this process usually takes significantly longer than with medical care. In addition, the body is usually very weak afterwards.
The prognosis worsens with resistant germs. These do not react to the medication and continue to multiply unhindered. Patients with a weakened immune system can experience serious complications in these cases. In the worst case, the pathogen cannot be killed and the patient dies as a result of the consequences.
prevention
Bacteremia can be prevented to the extent that the spread of bacteria into the blood can be prevented. In addition to disinfecting wounds, treating abscesses in good time is a preventive measure.
Aftercare
The best way to avoid bacteremia recurring is prevention. Patients should make sure they have a strong immune system. They achieve this through a balanced diet, physical activity and adequate sleep. If the immune system is already weakened, caution should be exercised with minor injuries.
Bacteria must not get into the bloodstream. It is advisable to protect the relevant areas with plasters or gloves. There is no immunity after bacteremia. Patients can get infected again and again. The diagnosis is made through a blood test. The doctor then orders drug treatment. Usually an antibiotic is used.
Complications threaten if the pathogen proves to be resistant to the active ingredients. Doctors then have to resort to unconventional methods. The main thing is to preserve vital organs. This does not always succeed. In the worst case, bacteremia can lead to death. If the symptoms worsen, it is advisable to visit the doctor again. The most important aspect is to prevent the spread of bacteria into the blood.
You can do that yourself
Untreated bacteremia can lead to sepsis and, in the worst case, septic shock with fatal outcome. The latter rarely occurs, but patients should always consult a doctor.
A healthy immune system usually prevents bacteria that penetrate the bloodstream from multiplying unhindered and from attacking vital organs. If there is an excessive concentration of bacteria in the blood, the immune system is usually weakened. A healthy lifestyle primarily contributes to strengthening the immune system.
This includes eating a plant-based diet rich in vitamins and fiber, and avoiding excessive consumption of alcohol, tobacco and refined sugar. Sufficient sleep and regular physical activity are also important. Light endurance sports such as swimming, cycling or walking are particularly beneficial.
Constant stress can also weaken the immune system and should therefore be avoided. In naturopathy, an active ingredient from the red coneflower (Echinacea Purpurea) is used to strengthen the body's own defenses.
Patients who already know that their immune systems are weakened should also take preventive measures. Bacteria can also get into the bloodstream through small injuries that are imperceptible to the person concerned. Gloves should therefore always be worn for risky activities. In everyday life, the preparation of (raw) meat is a risk factor that is often overlooked. Disposable gloves can protect against infections here.









.jpg)

.jpg)
.jpg)











.jpg)