The bacterial dysentery, Shigellosis or Shigella riot is a reportable infection of the intestine, which in its severe variant can lead to death in up to 10 percent of affected patients. This colon infection is caused by bacteria of the genus Shigella. The bacterial dysentery should not be confused with the amoebic dysentery, which is particularly common in travelers to tropical and subtropical regions.
What is bacterial dysentery?

© Kateryna_Kon - stock.adobe.com
In bacterial dysentery, there is an infestation with one of the four different Shigella species, whereby type A Shigella dysenteriae is the most severe form with a high death rate.
Bacterial dysentery leads to severe inflammation of the colon and, after an incubation period of two to seven days, causes severe diarrhea. There are up to thirty bowel movements per day, which severely weaken the patient.
Infection occurs through blood or urine and contact with contaminated objects, hands, water and food is sufficient. Since the Shigella bacterium is acid-resistant, the bacterial dysentery is not stopped by the stomach acid or the number of pathogens is reduced on the way to the intestine.
causes
The source of infection in bacterial dysentery is usually another sick person and their excretions. The bacterial dysentery is transmitted by smear infection. Only a few Shigella are sufficient for a new infection.
The bacterium passes through the stomach largely unhindered and finally reaches the colon, where in type A it produces a toxin that triggers bacterial dysentery. For bacterial dysentery, the hygienic conditions and health preconditions are an essential factor for the spread.
Bacterial dysentery spreads quickly and can only be contained again with considerable effort, especially in emergency situations after disasters, in which many people are together in a confined space under poor hygienic conditions. Physically weakened people, old people and small children are particularly at risk.
You can find your medication here
➔ Medication for diarrheaSymptoms, ailments & signs
The symptoms of bacterial dysentery are sudden and severe. Watery [[diarrhea] with abdominal pain, nausea] and vomiting usually occurs within the first two days of illness. Depending on which pathogen is the cause, the diarrhea either subsides without consequences or develops into bloody or slimy-purulent diarrhea. This is accompanied by complaints such as abdominal cramps, painful bowel movements and colic.
The loss of fluid manifests itself in impaired consciousness and external changes such as sunken skin, the edges of the eyes and torn corners of the mouth. Usually bacterial dysentery causes fever], which is characterized by sweating and other obvious symptoms. If the course is severe, shigellosis can cause severe pain.
In extreme cases, the intestine breaks through and blood poisoning occurs. The symptoms mentioned appear after one to two days in bacterial dysentery and subside within a week if the outcome is positive. Any complications delay the healing process and manifest themselves in a rapid increase in the feeling of illness. Most of the time those affected are very pale and no longer productive. The individual symptoms occur in shigellosis in different forms, but can clearly be traced back to the infectious disease.
Diagnosis & course
Characteristic of bacterial dysentery are initially watery, then slimy-bloody diarrhea, which is accompanied by collik-like abdominal pain as well as the painful urge to defecate and fever.Bacterial dysentery is initially made as a suspected diagnosis on the basis of these symptoms and possible external accompanying circumstances such as contact with people who are already sick.
A laboratory test for Shigella bacteria in the stool must be carried out for a reliable diagnosis. This separates bacterial dysentery from diseases with symptoms similar to salmonella infection or food poisoning. Once the diagnosis has been made, the responsible authorities are notified immediately, as bacterial dysentery is a notifiable disease under the Federal Disease Act.
Complications
Serious complications are rare in bacterial dysentery. In the absence of or inadequate treatment, however, the disease can cause various complications. The gastrointestinal complaints often lead to deficiency symptoms and dehydration, which in turn cause circulatory problems.
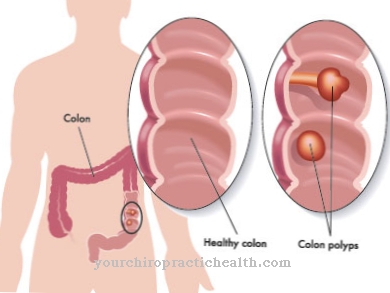
Shigellosis can also lead to the formation of cysts and ulcers in the large intestine, which often cause the intestines to expand. The intestinal wall rarely tears as a result, which can lead to life-threatening complications. Bacterial rest can also cause complications outside of the intestine: if the mucous membrane barrier in the intestine is damaged too much, other bacteria can establish themselves in the organism.
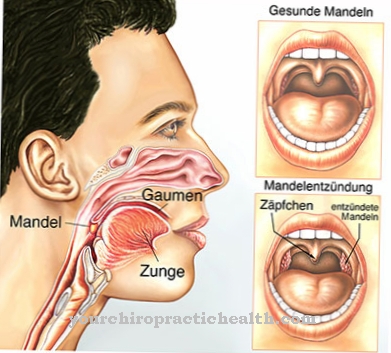
This can lead to Reiter's syndrome with inflammation of the conjunctiva, urethra and joints. Furthermore, dysentery can cause haemolytic uremic syndrome and increase the risk of arthritic joint changes. The typical symptoms of dysentery such as fever, abdominal cramps and colic can also lead to problems.
This is the case when the abdominal cramps promote the aforementioned damage to the colon. Young children, the elderly and patients with previous illnesses are particularly at risk for complications. In any case, bacterial dysentery should be clarified by a specialist.
When should you go to the doctor?
Bacterial dysentery is highly contagious and should therefore be treated immediately. The diarrheal illness can best be determined by the characteristic symptoms (fever, abdominal cramps, painful urge to defecate). If one or more of these symptoms appear after a long trip abroad (especially India, North Africa, and Turkey), it is likely bacterial dysentery. An immediate doctor's visit should then take place solely because of the obligation to report the disease.
If the bacterial dysentery remains untreated, it can also be severe and in rare cases lead to death. At the latest when circulatory problems occur or ulcers are noticed in the intestine, a doctor must be consulted. Patients with a chronic bowel disease or an immune deficiency should immediately discuss new or unusually severe symptoms with the responsible doctor.
Pregnant women, the elderly and children must also be examined quickly in order to avert a severe course. If physical or mental deficits are already noticeable, the emergency doctor must be called. In the event of circulatory collapse and coma, first aid measures must be provided until the rescue service arrives.
Doctors & therapists in your area
Treatment & Therapy
Regardless of the type of Shigella, bacterial dysentery is treated with suitable antibiotics. A distinction must be made between adults and children when choosing antibiotics, as some effective drugs are only approved for adults.
It should also be noted that bacterial dysentery quickly develops resistance and no longer responds to previously effective agents. In addition, the treatment depends on the general condition of the patient and the course. In the case of mild bacterial dysentery, treatment for bacterial dysentery is limited to the prescription of bed rest and a suitable diet. This applies to patients in a good general condition who can cope with bacterial dysentery on their own.
If there is also a large loss of fluid due to the diarrhea, the bacterial dysentery is treated with infusions. In the case of bacterial dysentery, it is important to strictly adhere to the hygiene regulations for patients and contact persons. Contaminated clothing and bed linen should only be touched with protective clothing and hands must be carefully disinfected before and after each contact. The spread of bacterial dysentery can thereby be contained.
Outlook & forecast
If bacterial dysentery is treated early, the chances of a cure are good and the symptoms of the intestinal infection will cease after about a week. Once the disease has been successfully overcome, those affected first have a temporary defense mechanism that protects them from being infected again. In lighter forms, the disease can even progress without any noteworthy symptoms.
The pathogens are transmitted with the stool. The symptoms then usually go away on their own approx. 4 weeks later. In some people, the bacteria settle in the large intestine for a long time and ensure that they infect other people without developing symptoms themselves.
Bacterial dysentery usually runs smoothly, but can lead to complications in people with a weakened immune system (children, the elderly, the chronically ill or people with an immunodeficiency). The persistent diarrhea caused by the loss of fluids and electrolytes can cause circulatory problems or even circulatory failure if the disease is not treated in time.
The inflammation of the intestinal lining can lead to ulceration, which can cause the intestine to dilate. In the worst case, the intestinal wall tears and can cause life-threatening complications.
You can find your medication here
➔ Medication for diarrheaprevention
Bacterial dysentery is an infectious disease that can only be prevented by particularly strict hygiene measures. People who are in affected areas must avoid any contact with the excretions of sick people or those who slowly recover. Appropriate protective clothing is important. For all other possibilities of infection, extensive hand washing before and after using the toilet reduces the risk of infection. However, bacterial dysentery cannot be completely ruled out.
Aftercare
The bacterial dysentery usually takes a good course. The disease heals completely. Re-infection is not possible for a limited time. The body has developed an immunity to the disease. Follow-up care to avoid a new infection is therefore usually not useful.
The situation is different for patients who frequently travel to warm countries with inadequate hygienic conditions. After the first appearance, you should ask your doctor treating you about everyday tips. Those affected bear a high degree of personal responsibility. One of the basic rules of conduct is not to eat food that has not been cooked.
Contact with flies can also promote bacterial dysentery. The disease can be transmitted through sexual contact, which is why follow-up care should also take third parties into account. If typical symptoms return, the doctor will examine a stool sample.
If “bacterial dysentery” is diagnosed again, it is important to compensate for the fluid loss due to the diarrhea. Antibiotics can shorten the progression of the disease and prevent complications. In principle, children and old people should exercise great caution in countries with poor hygiene standards. Your immune system is much more susceptible to infection with bacterial dysentery.
You can do that yourself
If you have bacterial dysentery, you should always see a doctor. Medical treatment can be supported by some self-help tips and home remedies.
The first thing you should do is adjust your diet. Food such as gruel, white bread, steamed vegetables and baby porridge protect the intestines and have a calming effect on the irritated intestinal flora. Sweet and fatty foods, alcohol and coffee, on the other hand, should be avoided. In general, flatulent foods, fatty fish and fatty meat should be avoided during the acute phase of the illness. In general, you should drink and eat enough to compensate for the loss of fluids and electrolytes.
Patients who are already in poor physical condition should also take dietary supplements and an appropriate fluid replacement. Alternatively, there are natural remedies. Blueberries or blackberries, for example, have a preventive effect against dysentery and cholera and can be taken either as tea or in the form of medicinal preparations.
Applications with sage, fennel and chamomile are just as effective. In consultation with the doctor, healing earth or Schuessler salts can also be tried. Finally, increased personal hygiene with regular hand washing helps to stop the spread of bacterial dysentery.


.jpg)

















.jpg)



