What is Buruli Ulcer?

© blueringmedia - stock.adobe.com
Buruli ulcer is a tropical disease caused by the bacterium Mycobacterium ulcerans. The bacterium develops a chronic skin infection with large ulcers. These often lead to distortion and subsequent stigmatization of those affected. The disease is estimated to be common in 30 African countries, but cases have also been observed in New Guinea or Australia. Around 20,000 people around the world are infected with the bacterium every year. Buruli ulcer affects children under the age of 15 in around 70 percent of all cases.
The World Health Organization (WHO) counts the disease as one of the neglected diseases. The ulcers are diagnosed too late and can often only be removed in a complicated operation. It is not uncommon for patients to be mutilated by the ulcers before diagnosis. That is why the WHO founded the Global Buruli Ulcer Initiative in 1998, which aims to raise awareness of the disease.
causes
As already mentioned, the cause of the Buruli ulcer is Mycobacterium ulcerans. It is a gram-positive, acid-fast and slowly growing rod bacterium. Mycobacterium ulverans is mainly found in humid tropical and subtropical regions. Standing water is probably the habitat of the bacterium. This is why people who live near lakes or in swamp areas are particularly affected. The transmission mechanism is not yet fully understood.
Transmission via mosquitoes is conceivable. In Africa, the pathogen was found in some mosquito species. Other small aquatic insects or a film of smear on the water may also be sources of infection. However, it is almost certain that the disease will not spread from person to person. In contrast to tuberculosis, which is also caused by a Mycobacterium, HIV-positive people do not seem to be particularly susceptible to Buruli ulcers.
Symptoms, ailments & signs
Mycobacterium ulverans produces the cell toxin mycolactone. This damages the tissue and at the same time weakens the immune system. A Buruli ulcer usually begins with painless swelling, lump formation, or hardening. There is no fever. The infection spreads on the surface of the skin and also eats into deeper and deeper layers of the skin.
Mycobacterium ulverans produces the cell toxin mycolactone. The pathogen destroys more and more tissue and large ulcers develop. The bacteria can even eat away at the bones. In spite of the ulcers, pain is rare, and even in the later course of the disease there is no fever due to the immunosuppressive effect of the pathogen toxin. The disease process can drag on for months to years.
Diagnosis & course
Buruli sufferers go to the doctor very late or not at all. There are mutliple reasons for this. Initially, the first symptoms are rather unspecific and are sometimes not even noticed. Then even the larger ulcers are usually not associated with pain. As a result, the disease is often not taken seriously, until it is usually too late for treatment.
But even if the patients suspect they are suffering from the tropical disease, they do not go to the doctor. Infection with Burili is a stigma, especially in Africa, and those affected suffer from marginalization. Therefore, the ulcers are often hidden under long clothing. The typical symptoms themselves provide decisive information for the diagnosis. In endemic areas, an initial diagnosis can be made directly in the field using a microbiological procedure, the Ziehl-Neelsen staining test.
The tissue material required is obtained from wound swabs. A newer and more specific method for the detection of pathogens is the PCR (polymerase chain reaction). Another way of making a diagnosis is by growing the bacterium in a culture. In order for a result to be found here, the infection must have occurred at least six weeks before the test was carried out. A prompt and early diagnosis is therefore not possible.
The most specific determination is possible with a histopathological examination of punch biopsied tissue. In most endemic areas, however, the necessary research material is not available.
When should you go to the doctor?
This disease definitely needs to be examined and treated by a doctor. There is no self-healing. As a rule, a doctor should be consulted if the person concerned has a significantly weakened immune system. There is swelling on the skin, but this is not associated with pain.
Fever can also indicate the disease. If various skin complaints suddenly arise, a doctor must be consulted in any case. Ulcers must also be examined to prevent further complications. In many cases the complaints are unfortunately very unspecific, so that no doctor is consulted. However, medical treatment is necessary in the event of long-term symptoms.
The diagnosis of the disease is usually made by a general practitioner or a dermatologist. For further treatment, however, the patients are dependent on the surgical removal of the affected skin areas. For this reason, a doctor should be consulted at an early stage to prevent scars.
Doctors & therapists in your area
Complications
As a rule, Buruli ulcer causes severe ulcers that can occur in different areas of the body. Most of the time, these spread to the patient's legs and, if left untreated, can lead to serious complications. There is usually swelling, which is initially painless.
As the Buruli ulcer progresses, pain and lumps on the skin develop. Hardening of the legs also often occurs. In the worst case, the pathogen penetrates directly into the lower skin layers and eats its way down to the bones. This can also severely damage the bones. Often those affected also suffer from a fever. The disease itself requires a relatively long treatment of about half a year.
The treatment is usually carried out with the help of a surgical procedure in which all of the affected tissue is removed. An amputation may also be necessary, in which the patient then suffers from severe restrictions in everyday life. Most of the time, the affected person still has to take antibiotics for a longer period of time after the operation. Apart from the scars from the operation, there are usually no further complications if the treatment is carried out early.
Treatment & Therapy
Since the Buruli ulcer is often diagnosed very late, the treatment of choice is usually the surgical removal of the infected tissue. However, with this method, relapses occur in 30 percent of cases, as bacteria have often already spread in tissue that appears healthy. Skin and tissue grafts may need to be used depending on the size of the ulceration. If the disease is very advanced, the only thing left to do is amputation of the affected limb.
In addition to the surgical removal of the pathogen and the infected areas, the World Health Organization recommends eight weeks of therapy with special antibiotics. This can reduce the recurrence rate to two percent. In many cases, however, functional restrictions and large scars remain. The disease rarely heals without treatment.
Outlook & forecast
In many cases, the prognosis for Buruli ulcer is unsatisfactory. In principle, the disease can be cured, but this requires a very experienced team of doctors because the treatment is very complicated and lengthy. Serious consequences can only be avoided by combining intensive wound care, antibiotic treatment and surgical interventions. Although the disease is rarely fatal, it can lead to loss of limbs and severe joint stiffness, which ultimately leads to restricted mobility.
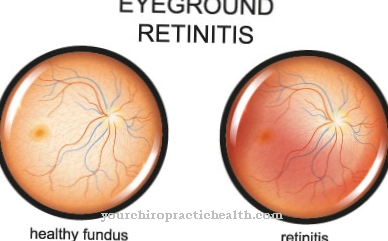
Without treatment, the responsible bacterium Mycobacterium ulcerans destroys the subcutaneous tissue. Progressive ulcers penetrate to the bones and muscles and destroy them. Since the defense cells of the immune system are also attacked, the bacterium can survive in the body and further destroy the affected tissue. The ulcers take many months or even years to stop. Uncontrolled scarring of entire parts of the body forms, which among other things can lead to deformation of the limbs and other parts of the body or even to loss of eyes. Furthermore, the risk of secondary infections increases, which in severe cases can be fatal.
Often the only option left is to surgically remove affected tissue to prevent the disease from spreading. Limb amputation is also sometimes necessary. Serious complications of the ulcers are shrinkage and stiffening of the joints, which later have to be treated by plastic surgery.
prevention
Buruli disease cannot currently be prevented. According to the WHO, the Bacillus Calmette Guérin vaccination (BCG), which is actually used for tuberculosis prophylaxis, offers short protection against Mycobacterium ulcerans. Longer-term protection could only be achieved with a special vaccine against Buruli. This vaccine is currently being researched.
Aftercare
The Buruli ulcer always requires extensive follow-up care after drug and surgical treatment. After the surgical treatment, the affected skin area must be protected from pathogens and other external influences. The bandage can be removed after a few days in consultation with the doctor.
The doctor will check that the wound has healed as expected a few days after the operation. If no complications are found, no further follow-up checks are normally required. However, if the wound does not heal as expected, the doctor will need to do further tests.
A change in medication is often necessary or the operation has to be repeated because the infection has not completely subsided. If the course is complicated, further check-ups are necessary. The patient has to visit the dermatologist once or twice a month so that the necessary examinations can be carried out.
In addition, other doctors must be involved, as a repeated occurrence or a complicated course of the Buruli ulcer indicates a serious underlying disease. Good wound care is also part of aftercare. The patient should contact the doctor after the treatment is completed so that the necessary measures can be initiated.
You can do that yourself
A Buruli ulcer is often diagnosed late and must always be removed by chemotherapy or surgically. Surgical or chemotherapeutic intervention puts a great strain on the affected organism, which is why those affected must pay particular attention to good preparation and follow-up care.
In preparation for the operation, the medical guidelines must first be observed. Usually an adapted diet is suggested, especially shortly before the procedure, no luxury foods or overly fatty foods should be consumed. Patients who take medication regularly should tell the doctor about it. Usually the medication does not need to be adjusted, but if you have a heart condition, at least a check-up is indicated.
After the operation, rest and bed rest are indicated. The affected person should also make sure that the wound is well cared for. Otherwise, pathogens can get into the wound and cause serious complications. If unusual symptoms develop, the doctor must be informed immediately. In general, good monitoring by the doctor is indicated in the case of a Buruli ulcer, as the tropical disease can occur weeks or months after the diseased tissue has been removed.

.jpg)

.jpg)


















.jpg)



