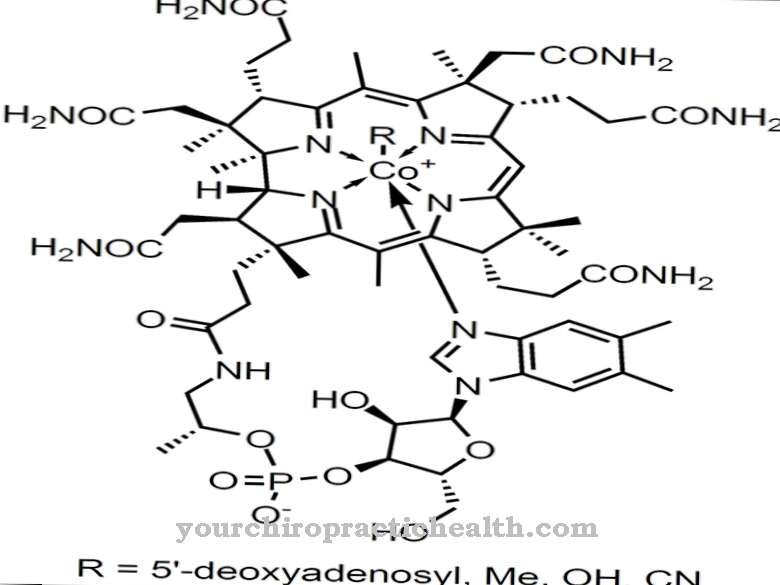
Calcitonin is a 32 amino acid polypeptide that is mainly produced in the C cells of the thyroid gland. As a controlling hormone by inhibiting bone breakdown and by increasing the excretion of calcium and phosphate, it lowers the calcium and phosphate level in the blood. With regard to calcium concentration, calcitonin is an antagonist and with regard to phosphate concentration, the protagonist of parathyroid hormone.
What is calcitonin?

Calcitonin is a 32 amino acid polypeptide that acts as a control hormone in the body's calcium and phosphate balance. A high calcitonin level, by inhibiting the osteoclasts, lowers the supply of calcium from the bone breakdown process, which leads to a rapid decrease in the calcium level in the blood.
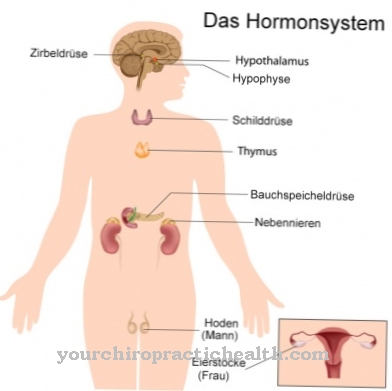
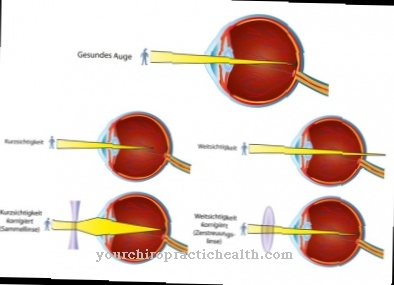
In terms of calcium concentration, it has an antagonistic effect and, in terms of phosphate concentration, protagonistic of the parathyroid hormone, which is mainly synthesized in the parathyroid glands. As the “third party”, vitamin D also plays an important role in the control cycle of the calcium and phosphate balance. An increase in vitamin D levels causes an increase in calcium and phosphate levels in the blood.
Calcitonin is therefore an antagonist to vitamin D. Vitamin D can also inhibit the synthesis of parathyroid hormone. Calcitonin only has a physiological half-life of a few minutes and therefore quickly loses its effectiveness as soon as the incentives for further synthesis cease, e.g. B. after normalization of calcium levels.
Production, Education & Manufacturing
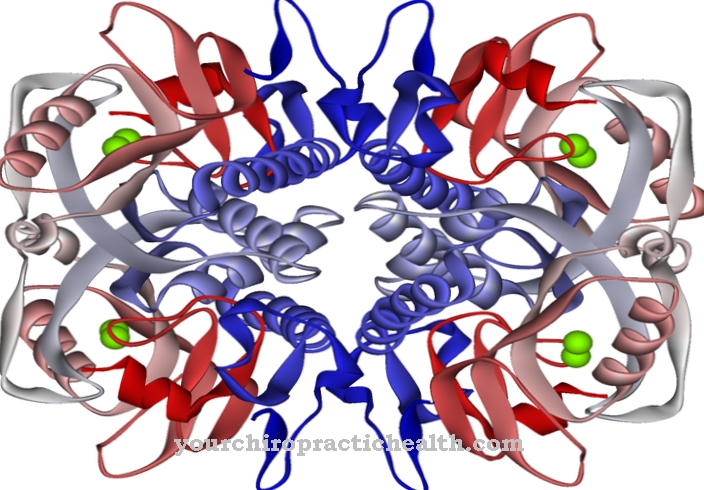
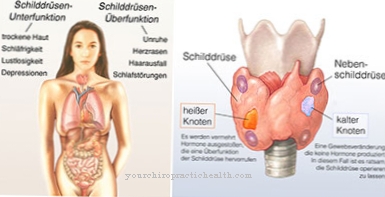
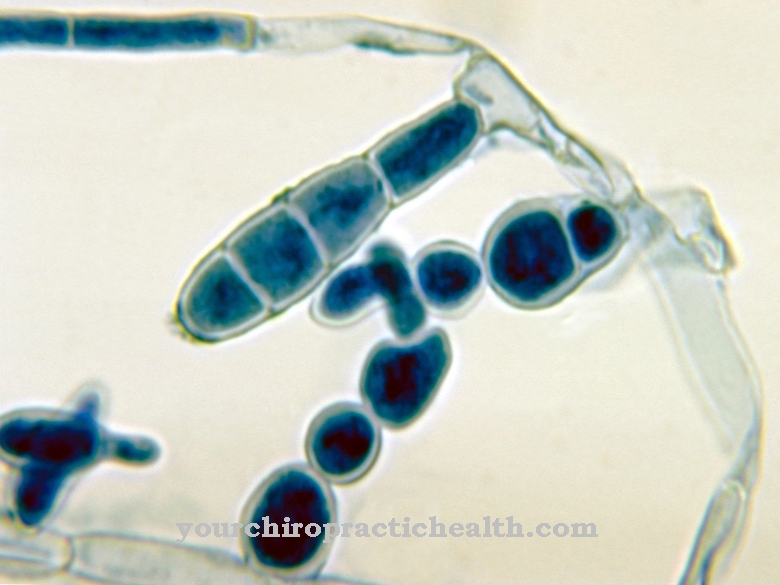
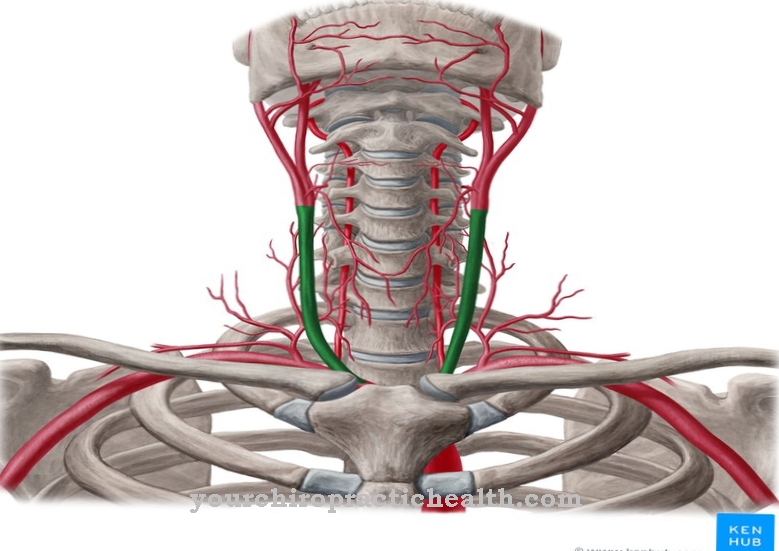
Calcitonin is mainly synthesized in specialized parafollicular cells (C cells) of the thyroid gland when needed. In part, calcitonin can also be produced in the parathyroid glands and thymus, e.g. this is very important after a necessary complete removal of the thyroid gland.
As a further compensation in the event of a thyroid failure, the motor and sensory nerve cords of the peripheral and central nervous system are also able to contribute the glandotropic calcitonin gene-related peptide (CGRP), which has a similar effect as calcitonin. The synthesis of calcitonin is stimulated by a (too) high concentration of calcium ions in the blood serum.
The hormone production also responds to stimulation by certain gastrointestinal messenger substances. The short physiological half-life ensures that when a normal calcium concentration in the blood serum is restored, the effectiveness of the calcitonin decreases very quickly through natural degradation.
Function, effect & properties
Calcitonin influences several physiological processes at the same time. If the calcium concentration in the blood serum rises above normal, the C cells in the thyroid are stimulated to produce calcitonin.
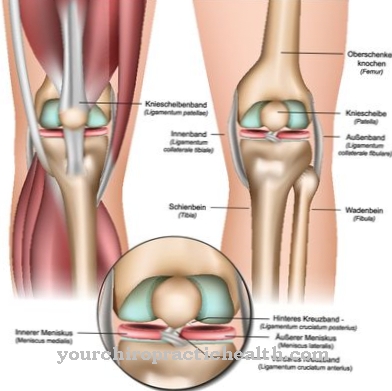
The main effect of the now produced calcitonin is the inhibition of the osteoclasts, which as opponents of the osteoblasts constantly break down bone cells and "recycle" the substances they contain, such as calcium and phosphate. This releases calcium and phosphate, which are briefly available in the blood serum - and, to put it simply - can be used again by the osteoblasts for building bones at the same or another location.
If the breakdown process of the osteoclasts is inhibited and the osteoblasts continue to build the bone without being disturbed, an imbalance quickly arises between the breakdown and build-up process in favor of build-up or in favor of higher “consumption” of calcium and phosphate. This will lower the calcium and phosphate levels as intended. At the same time, calcitonin stimulates an increased excretion of calcium in the [kidneys]] and in the intestine.
The calcitonin-like CGRP, which is also synthesized, also has an appetite-suppressing effect, slows down gastric acid production and leads to a number of other physiological processes such as an increase in the pulse rate and expansion of the blood vessels. It stands to reason that calcitonin is also used as a drug to use the effect of inhibiting bone loss for therapeutic purposes, especially in advanced osteoporosis or in Paget's disease with visible bone deformations or pathologically elevated calcium levels.
It must be taken into account that calcitonin, as a polypeptide, would be digested immediately if taken orally before it could take effect. Only parenteral forms of administration are therefore possible, such as subcutaneous or intravenous. Administration as a nasal spray in women to prevent postmenopausal osteoporosis was stopped again in 2012 because of possible serious side effects.
Illnesses, ailments & disorders
If the calcium level in the blood is normal, it is more normal that the calcitonin values are very low, possibly even below the detection limit. The definition of a minimum value therefore makes no sense, only if there is also an excessive calcium level.
A pathological hypofunction can therefore hardly be proven, since it would have to be coupled with an increased calcium level at the same time. If increased calcium concentrations persist and are not normalized by the body's own calcitonin, it is hypercalcemia (also hypercalcemia), which may indicate a serious illness.
Non-treatment can lead to neuromuscular and intestinal symptoms and, in the medium term, to renal insufficiency, heart failure and death. A pathological hyperfunction of the C-cells can be proven and can be interpreted as a tumor marker for a C-cell carcinoma (medullary thyroid carcinoma) or for a C-cell hyperplasia, in which the C-cells autonomously produce calcitonin and respond to the stimulating hormones or the Calcium levels in the blood stop responding.
High calcitonin levels can also indicate cirrhosis of the liver, kidney failure, or a neuroendocrine tumor.











.jpg)




.jpg)


