Chronic Pelvic Pain Syndrome (CPPS) describes chronic pelvic pain syndrome, a disease that is difficult to treat. A combination of different factors is what causes the symptoms that are associated with it.
What is Chronic Pelvic Pain Syndrome?
Chronic Pelvic Pain Syndrome, the chronic pelvic pain syndrome, is a painful condition in the pelvic area. Men in particular are affected by the disease. In the past, the complaints were grouped under the painful prostate (prostatodynia). The Chronic Pelvic Pain Syndrome (CPPS) is an insidious disease as treatment so far has proven difficult.
causes
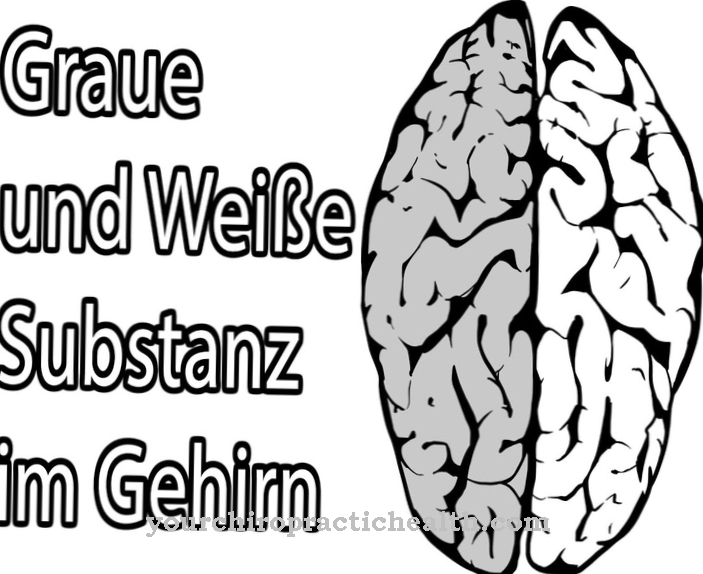
One of the causes of Chronic Pelvic Pain Syndrome (CPPS) is vegetative dysregulation that is triggered by stress. Due to a venous congestion of the venous plexus, which are stored around the prostate, it happens that the accompanying sensitive nerves are irritated. The pain and abnormal sensations lead to symptoms.
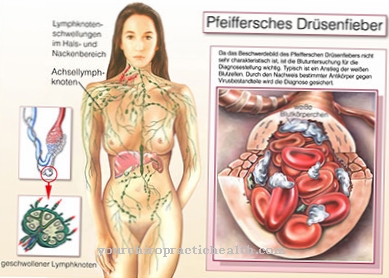
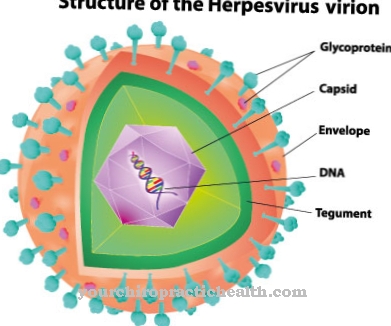
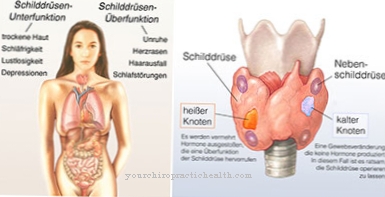
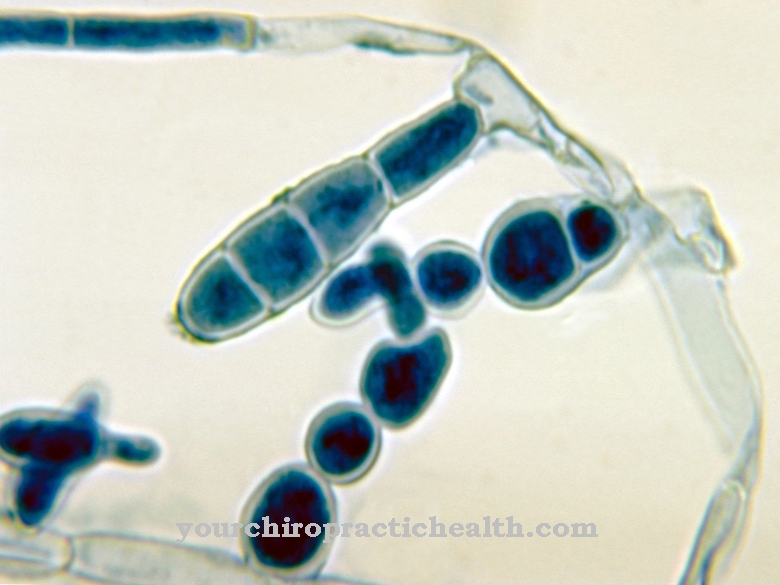
According to an American study, the symptoms of Chronic Pelvic Pain Syndrome (CPPS) are based on an interplay between mental factors and a dysfunction in the immune system. This includes, for example, dysregulation of the local nervous system resulting from previous trauma or infection.
This causes those affected to tense up the pelvic area due to suppressed feelings of fear, which can lead to more and more inflammation. The reason for this is that the nerves in the pelvic area are chronically activated. Cold is also suspected as a possible trigger or intensifier for Chronic Pelvic Pain Syndrome (CPPS). Many sufferers feel relief as soon as heat is applied to the affected area.
You can find your medication here
➔ Medicines for painSymptoms, ailments & signs
.jpg)
© nerthuz - stock.adobe.com
Chronic Pelvic Pain Syndrome (CPPS) causes pelvic pain, but it does not result from an infection of the urinary tract. Symptoms may increase or decrease and the pain may be mild or very severe. In the latter case, it is often no longer even possible to assume a normal sitting posture.
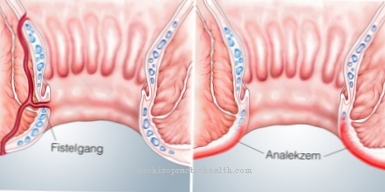
Other signs are often difficult urination, a frequent need to urinate, pain in the joints and muscles, tiredness, abdominal pain, a burning sensation in the penis, pain after ejaculation as well as itching, stinging and cramps in the anus.
These symptoms can appear individually or in combination. Depression, withdrawal from the social environment, problems in the partnership and discouragement are possible due to the chronic pain condition and the heavy burden of the Chronic Pelvic Pain Syndrome (CPPS). This can even go as far as occupational disability and addiction.
Diagnosis & course
There are currently no definitive tests to clearly diagnose Chronic Pelvic Pain Syndrome (CPPS). Pressure pain can usually be triggered at the lower testicle or the opera pole. An inconspicuous and non-pressure-sensitive prostate is palpated through the anus (rectal). The kidney beds are free from pounding pain on both sides.
Doctors also use digital rectal scanning of the prostate. This is followed by a 4-glass sample (first urine, midstream urine, prostate secretion and the urine after a prostate massage) to localize the bacterial pathogen. Other diagnostic methods are the analysis of the ejaculate, ultrasound (sonography) or uroflowmetry to determine functional or anatomical urinary flow disorders.
Chronic Pelvic Pain Syndrome (CPPS) usually subsides slowly over several days to weeks. However, it can recur due to adverse circumstances or reloading.
Complications
As a rule, chronic pelvic pain syndrome is a disease that is difficult to cure. The syndrome usually causes severe pain in the patient, especially in the pelvis. The pain itself can also take the form of pain at rest and often prevents the person affected from adopting a healthy and habitual sitting posture.
There is also pain in the joints and muscles. The patient also suffers from a tiredness that cannot be compensated for with the help of sleep. When urinating, there is a burning sensation and pain, the pain can also occur during ejaculation and have a negative effect on sex life.
Often those affected also suffer from psychological complaints and depression as a result of the symptoms. Social contacts are severely limited. In many cases, the patient can no longer pursue employment. The treatment of Chronic Pelvic Pain Syndrome is primarily aimed at reducing pain.
Many patients also need psychological counseling, which can be supported with the help of medication. There are no further complications, but the Chronic Pelvic Pain Syndrome extremely restricts the patient's life and leads to a greatly reduced quality of life.
When should you go to the doctor?
In the case of chronic pelvic pain, fatigue and frequent urination, a doctor should always be consulted. The symptoms are usually based on a serious illness that must be clarified by a doctor and treated if necessary. A digital rectal scan of the prostate and some other tests can determine whether the underlying condition is Chronic Pelvic Pain Syndrome. If the diagnosis is made, comprehensive medical treatment is indicated. The person concerned should consult the doctor regularly and inform him about unusual symptoms.
Should psychological complaints such as depression or anxiety disorders arise, a therapist can be consulted in consultation with the doctor. For chronic pain, relaxation therapy is also helpful to reduce physical and mental stress. Nocturnal pelvic pain and possible accompanying symptoms such as cramps in the anus, joint and muscle pain or itching are a case for the medical emergency service. In the event of severe complaints, the person affected should be taken to the nearest clinic for further clarification.
Doctors & therapists in your area
Treatment & Therapy
After other malfunctions have been ruled out, heat has an immediate effect. This can be a hot water bottle or a hot hip bath. Increased movement is also helpful, although no pressure should be exerted on the perineum, as is the case, for example, when cycling.
The intake of pumpkin seed and grass pollen extracts has also proven itself.A pelvic floor exercise is also a good way to slowly learn to use the muscles correctly again. This can be done using electrical stimulation, which uses a probe to apply a painless current to the tense areas and thus can help reduce pain. These devices are available for home use and are very easy to use.
Since fear or panic can also be the trigger for Chronic Pelvic Pain Syndrome (CPPS), psychological treatment and relaxation therapy are also helpful to reduce the stress level. Acupuncture and drug treatment can also help improve symptoms, with alpha blockers appearing to have the greatest effect. Successes have also been observed with antibiotics, even if this type of treatment is controversial.
Outlook & forecast
Chronic Pelvic Pain Syndromes have an unfavorable prognosis. The cure of the disease is considered difficult and is not achieved in a large number of patients despite great efforts. It often takes many years to make a diagnosis from the initial manifestation. In many cases, the patient has already consulted several doctors and had numerous examinations carried out. Since there are no specific tests for recognizing Chronic Pelvic Pain Syndrome, it is much more difficult to diagnose the disease. This delays the start of treatment.
In addition to the complaints and the immense emotional challenges in dealing with the disease, there are often secondary effects. These worsen the chances of recovery and lengthen the path of recovery. Nevertheless, the symptoms can be alleviated.
In addition to drug treatment, emotional and mental strengthening is of great importance. With an optimistic basic attitude towards life, the reduction of the stress experience and a stable psyche, an improvement in health is given.
The symptoms can vary in intensity. In addition, episodes are possible in which there is hardly any impairment or in which there is no symptom. Often times, symptoms gradually decrease over several days until the patient is free from pain or other impairment. However, a recurrence in challenging times is very likely.
You can find your medication here
➔ Medicines for painprevention
Everyone reacts differently to stress. How pronounced this is depends on the physical and mental state of the person concerned. The more balanced and healthy a person is, the lower the risk of developing Chronic Pelvic Pain Syndrome (CPPS).
It is therefore very important to avoid stress as much as possible so that the pelvic area is not tensed again and again, which often happens unconsciously. The same applies to avoiding the cold, as this could also be identified as a trigger. Many sufferers get good relief from their symptoms as soon as they feel warmth in the relevant areas.
Long-term stabilization of Chronic Pelvic Pain Syndrome (CPPS) can generally be achieved through a healthy diet, an optimal lifestyle and sufficient periods of recovery, as the disease usually results from a combination of various unfavorable factors.
Aftercare
As a rule, chronic pelvic pain syndrome cannot be treated completely, so that the options for follow-up care are very limited in most cases. The affected person is primarily dependent on an early diagnosis so that there are no further complications or further worsening of the symptoms.
The earlier the Chronic Pelvic Pain Syndrome is recognized, the better the further course is usually. With this disease, a lot of exercise can have a positive effect on the symptoms. In general, the person concerned should lead a healthy lifestyle and eat healthily. Sports activities that challenge the entire body are also very useful and can alleviate the symptoms.
Physiotherapy measures can also be used, whereby many exercises from such therapy can also be performed in your own home. In some cases, medication is also required to treat chronic pelvic pain syndrome. If antibiotics are taken, it should be noted that they are not combined with alcohol. Typically, chronic pelvic pain syndrome does not reduce the patient's life expectancy.
You can do that yourself
According to the current state of knowledge, the Chronic Pelvic Pain Syndrome (CPPS) results from a combination of psychological factors and an impairment of the immune system. The main cause is constant stress, as those affected tend to tense the pelvic area a lot in this emotional situation, which leads to inflammation that does not heal properly or occurs again and again.
The best means of self-help is therefore to avoid fear, stress and other exceptional emotional situations that can lead to tension in the pelvic area. It is not always possible. Affected people can learn to cope better with stress. A number of relaxation techniques are available for this.
The most common are yoga and autogenic training. Corresponding courses are now also regularly offered by adult education centers in small towns. In all major cities there are institutes or freelance teachers who introduce those interested in these techniques.
Most sufferers use warmth during acute attacks. Warm full or hip baths are particularly helpful. Chemical hand warmers, which can be placed inconspicuously in underwear and then warm the pelvic area, are helpful for traveling or for acute attacks at work.
Some sufferers also benefit from natural history treatment methods such as taking pumpkin seeds or traditional healing methods such as acupuncture.

.jpg)
.jpg)






.jpg)





.jpg)