Clostridia are bacteria that form a family of their own. They cause different diseases, most of which are treated with antibiotics. Other therapeutic approaches that promise long-term success are changing one's diet and adding prebiotics and probiotics.
What are clostridia?
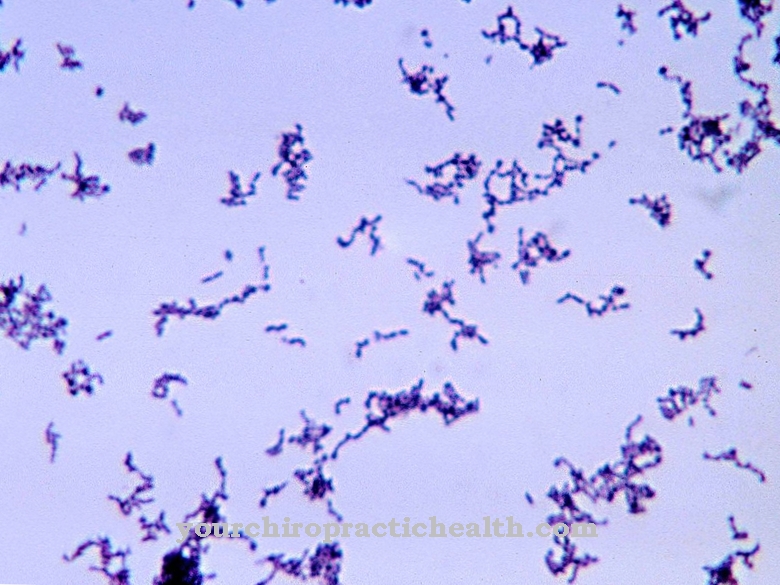
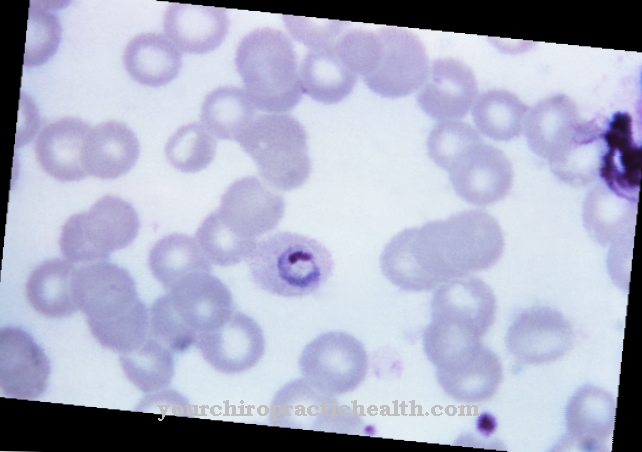
Clostridia are gram-positive anaerobic rod bacteria that - depending on which Clostridium bacterium it is - can cause different diseases in humans and animals. Clostridium difficile, for example, is present in smaller numbers (around 5%) in the intestines of every healthy adult without causing problems. However, if antibiotics such as erythromycin and clindamycin for another disease kill the health-promoting intestinal bacteria, the clostridia multiply quickly. They are resistant to many antibiotics.
Most clostridial species cause disease. The non-pathogenic species are now used in biotechnology. The rod bacteria are categorized into three groups according to their diet: The proteolytic clostridia break down proteins, Clostridium acidi-urici, for example, breaks down uric acid. The saccharolytic bacteria ferment carbohydrates such as starch, cellulose and sugar into acetone, butyric acid, carbon dioxide and molecular hydrogen (H2).
Hospital patients, people over 65 years of age, immunocompromised people (HIV patients, cancer patients who receive cytostatics), patients who take proton pump inhibitors (PPIs) and people who have been malnourished for many years (too many carbohydrates, fats, animal proteins) are particularly at risk from clortridia ) have a disturbed intestinal flora.
Occurrence, Distribution & Properties
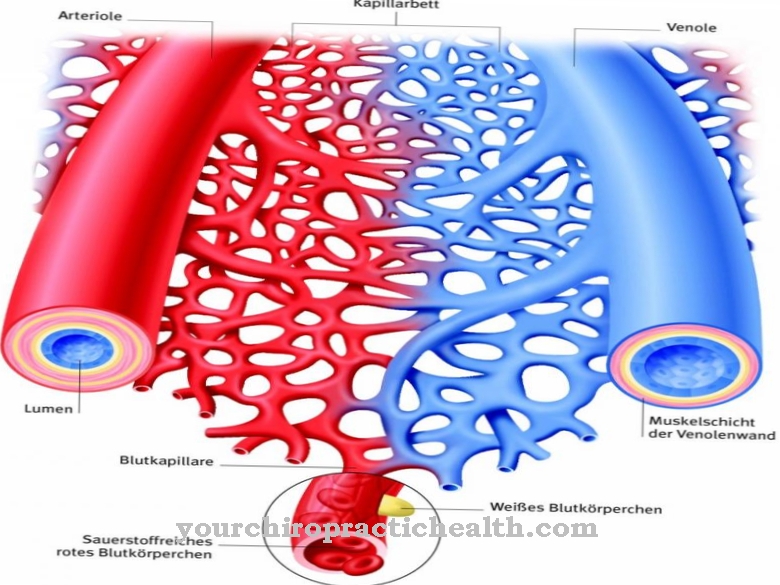
About 5% of the clostridia are found in the intestines of healthy adults without causing damage. In infants, the proportion of rod-shaped bacteria is around 80% compared to other intestinal bacteria. In the form of spores, the clostridia can survive for many years in the soil and in near-surface water. With the exception of Clostridium perfringens, all Clostridia species have a flagella, which the anaerobic, gram-positive bacteria can use to move. The bacteria are sensitive to heat, drought and certain chemicals (disinfectants). However, the spores are insensitive to heat and can withstand high sterilization temperatures, for example in the production of food, undamaged. They get into food through contamination with dust and soil, spoil them and, for example, swell up cans of food.
Since the clostridial spores, in contrast to the bacteria, can survive well in an oxygen-rich environment, they colonize door handles, toilet seats, towels, etc. and can repeatedly cause new intestinal diseases in people. They are transmitted from person to person via insufficiently washed hands after a bowel movement. Even small amounts of bacteria or spores are sufficient. Other types of clostridia, such as Clostridium botulinum, are inactive after just 30 minutes' heating at 80 degrees Celsius.
Illnesses & ailments
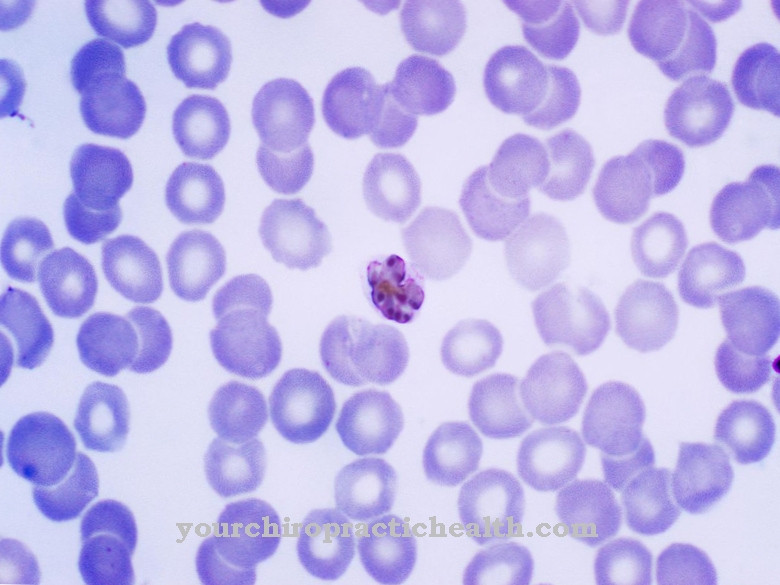
Clostridium difficile causes severe contagious diarrhea in hospital patients: the bacteria produce the toxins enterotoxin A and B, which attack the walls of the colon and lead to the formation of pseudomembranes. This leads to an increased excretion of electrolytes and fluids from the intestine. This form of reportable colitis is usually caused by ingestion of antibiotics, which kill much of the healthy intestinal flora.
The first signs can already be recognized 4 to 9 days after the first antibiotic intake: diarrhea, abdominal cramps, nausea, in severe cases also fever and bloody stools with a foul odor.
In the worst case, hospitalized patients experience enlargement of the large intestine, intestinal obstruction, intestinal wall tears and blood poisoning. A particularly virulent variant of Clostridium difficile, ribotype O27, was recently discovered in Germany. It often causes fatal intestinal infections.
Antibiotic-induced colitis can be treated well with metronidazole or vancomycin. Infusions balance the electrolyte balance that was disturbed by the diarrhea. In addition, patients have to drink a lot.
The intestinal infection is treated naturopathically with prebiotics and probiotics. In rare cases, the colitis will go away on its own. A total of 6 out of 10 patients have a good chance of a complete cure. After the symptoms have subsided, they excrete Clostridium pathogens in their stool for a few days. The rapid stool test or a culture of bacteria from the patient's stool reveal whether a patient has an infection with Clostrium difficile.
Clostridium botulinum excretes botulinum toxin (Botox), a nerve poison that is used in cosmetic surgery for injections into wrinkles. Clostridium tetani causes tetanus (tetanus). Clostridium perfringens causes type A food poisoning and gas fire. Other rod bacteria of the Clostridia family are responsible for other types of gas blight, intoxicating blight (in sheep and cattle), smoky fire and abomasum parasitic blight. Clostridium perfringens, for example, secretes the enzymes phospholipase and lecithinase, which destroy the cell walls. It feeds on fats and proteins, which it metabolizes into hydrogen sulfide, biogenic amines and other substances. The biogenic amines are considered to be the cause of colon cancer. The patient receives metronidazole for treatment and, for example, charcoal tablets for diarrhea. Healing clay (bentonite) and charcoal tablets can bind the toxins so that they are excreted in the stool. It is also advisable to rebuild the healthy intestinal flora.
Because all Clostridium species and their spores are highly contagious, infected hospital patients are immediately isolated. They stay there up to three days after their infection heals. The only way to prevent the transmission of the spores is to wash your hands frequently with soap and water. Then the hands should be dried well. Alcoholic hand disinfection is ineffective. Sodium hypochlorite and peracetic acid are suitable for surface disinfection.











.jpg)



.jpg)

.jpg)