Of the Cushing reflex is basically not a real reflex, but a connection between intracranial pressure, blood pressure and heart rate. As intracranial pressure rises, blood pressure rises to keep the brain supplying oxygen. The perfusion pressure in the brain corresponds to the difference between mean arterial pressure and intracranial pressure.
What is the Cushing Reflex?

In 1901, the American neurologist Harvey Cushing discovered a connection between the increase in intracranial pressure, the decrease in heart rate and the increase in blood pressure. The context has been named in his honor since it was first described and is therefore referred to as the Cushing reflex.
The formula of the reflex is CPP = MAP - ICP. ICP stands for intracranial pressure (brain pressure), MAP stands for mean arterial pressure and CPP for partial brain pressure. In other words, the perfusion pressure in the brain is made up of the difference between the mean arterial pressure and the intracranial pressure. The latter opposes the arterial pressure and is overcome by it as resistance.
Sometimes instead of the Cushing reflex there is also the Cushing triad the speech, which consists of hypertension, bradycardia and irregular, inadequate breathing.
In the true sense, the increase in blood pressure and the decrease in heart rate after an increase in intracranial pressure is not a real reflex with a reflex arc.
Function & task
Increases in intracranial pressure can be due to a number of factors. For example, masses of the brain parenchyma can increase the pressure, including a brain tumor. The same applies to any swellings in the brain, such as those in the form of cerebral edema. Brain edema is often the result of a traumatic brain injury.
In addition, strokes and inflammation can increase intracranial pressure in the brain. Other causes are increases in the volume of the liquor, as is the case with disorders of the drainage of the cerebral fluid.
If the intracranial pressure rises because of one of the phenomena just described, the perfusion pressure of the brain automatically falls. Because of this, the brain receives less blood. The blood transports vital oxygen to the brain. Therefore, when the perfusion pressure falls, the nerve cells are no longer adequately supplied with oxygen and there is a risk of irreversible damage to the nerve tissue.
The body wants to prevent this. The organism therefore tries to keep the mean arterial and intracranial pressure at a certain constancy. To do this, the body greatly increases blood pressure. Increases in systolic blood pressure of up to 300 mmHg are to be expected. As blood pressure increases, so does ICP. This causes the arterial pressure to rise even higher. At the same time, the heart rate drops. Because the organ has to recover from the increased stress. The pressure pulse arises on the basis of these relationships; it is caused by a suddenly increased sympathetic activity in the medulla oblongata.
Self-regulation of blood pressure can be expected after a certain time. Therefore, the administration of antihypertensive drugs is contraindicated in the situation described. The doctor only has to lower the systolic blood pressure to below 160 mmHg if there is active bleeding into the brain, such as a ruptured aneurysm.
In summary, the Cushing reflex describes the falling perfusion pressure, the decrease in cerebral blood flow and the compensatory measures of systemic increase in blood pressure, which are carried out by the body after an increase in intracranial pressure in order to keep the MAP-to-ICP ratio constant. The subsequent increase in the ICP increases the arterial pressure again, thus creating a vicious circle.
Illnesses & ailments
The Cushing reflex gains clinical relevance with all increases in intracranial pressure and can therefore be relevant in the context of bleeding, CSF disorders, strokes, edema formation, after trauma or in tumors.
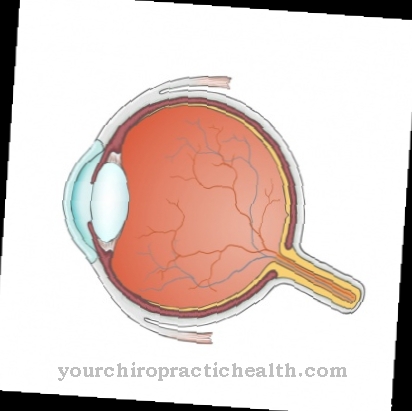
Signs of increased intracranial pressure include symptoms such as more or less severe headache, vomiting or edema within the optic nerve papilla. The edema can be diagnosed using an ophthalmoscope.
If several of the symptoms are present at the same time, there is a so-called intracranial pressure triad. The triad is often associated with side effects such as dizziness, paralysis of the eye muscles, bradycardia or breathing and impaired consciousness. An absence up to a coma can occur in the context of increased intracranial pressure. Most of the time, the patients suffer more from agitation and experience a general rise in blood pressure and a drop in heart rate as part of the Cushing reflex.
Patients with high intracranial pressure are monitored by intensive care medicine and placed in bed with their upper bodies raised by 30 or 45 degrees. Your head must be as straight as possible so that the venous drainage can take place without obstruction. With slight hyperventilation, the blood vessels narrow. In this way, a slight reduction in ICP can be achieved therapeutically.
Further treatment depends on the cause of the increased pressure. Edema can be resolved or reduced by administering diuretics. In the event that the autoregulation does not take effect with regard to blood pressure in the brain, patients with increased intracranial pressure are closely monitored with regard to their blood pressure. Invasive blood pressure measurements are often used for this purpose. In this way, if the Cushing reflex is absent, intervention can be made. Various drugs are available for intervention, which can maintain the blood pressure physiologically and in this way, on the one hand, have an effect on the intracranial pressure and, on the other hand, can ensure the blood supply to the brain tissue. Increased intracranial pressure can be a life-threatening situation.























.jpg)



