The diabetic retinopathy is damage to the retina of the eye (retina) caused by the metabolic disease diabetes mellitus.
What is Diabetic Retinopathy?

© logo3in1 - stock.adobe.com
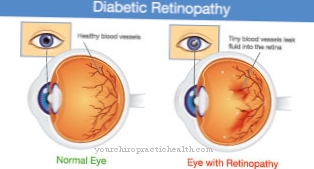
Diabetic retinopathy is a secondary disease of the diabetes mellitus disease. Diabetes mellitus damages the smallest arterial blood vessels through deposits and scarring, so that it comes to circulatory disorders in the affected organs (e.g. in the eye) (microangiopathy).
If the retina is damaged by scarring, the eyesight is impaired, which can lead to blindness. Diabetic retentionopathy, which causes 30% of all blindness cases in Europe, is the most common cause of blindness in people between 20 and 65 years of age.
About 90% of all type 1 diabetes and about 25% of all type 2 diabetes sufferers also suffer from diabetic retinopathy after 15 to 20 years of diabetes mellitus disease. The first eye changes occur on average after 10 to 13 years. Diabetic retinopathy leads to blindness in every fiftieth diabetic.
causes
The main cause of diabetic retinopathy is a long-standing diabetes mellitus disease. The risk of diabetic retinopathy increases with poorly controlled blood sugar levels. The occurrence of diabetic retinopathy or its further development can be avoided or at least delayed if the blood sugar is strictly controlled.
In phases of life that are characterized by hormonal changes (e.g. puberty or pregnancy), the risk of developing diabetic retinopathy is also increased. There is an additional risk of disease during pregnancy if the blood sugar is poorly controlled, if the blood sugar is adjusted too quickly in the early phase of pregnancy and in preeclampsia associated with high blood pressure (hypertension).
In general, hypertension, hyperlipidemia (increased blood lipid levels) and damage to the kidneys caused by diabetes favor diabetic retinopathy.
Symptoms, ailments & signs
This disease causes various symptoms of the eyes. Since the disease usually always occurs as a result of diabetes, those affected also suffer from diabetes. First and foremost, there are various visual disturbances and, in general, poor eyesight. The patients are therefore dependent on wearing a visual aid in their everyday life and therefore suffer from restrictions in everyday life.
When seeing, black points can also appear in the field of vision, which cannot be easily removed. Bleeding also occurs in the vitreous itself, which can also impair vision. If left untreated, the disease will eventually lead to complete blindness. This cannot be reversed.
Children in particular can suffer from sudden and irreversible visual problems, which can lead to depression or other psychological impairments. The infection can spread to the rest of the body if left untreated. The kidneys and heart are also attacked, so that these organs can also be permanently damaged. Without treatment, the patient's life expectancy is significantly reduced. In some cases, patients also suffer from delayed wound healing.
diagnosis
If diabetic retinopathy is suspected, an ophthalmoscopy (funduscopy, reflection of the fundus of the eye) is performed to examine the blood vessels of the retina. With the direct funduscopy, the vascular starting points in the center and the “yellow point” (macula) with the greatest density of visual cells are checked using a concave mirror or a converging lens.
In the case of indirect fundoscopy, the magnification is somewhat lower, but the examining doctor has a better overall view, which also includes the periphery of the retina and enables a three-dimensional assessment.
The imaging method of fluorescence angiography is also used to examine the fundus. In this case, dyes such as indocyanine green or fluorescein are injected intravenously in parallel to the drug-induced dilatation of the pupil. What is of interest for the examination is how quickly the dyes used as contrast media reach the retina and how they are distributed there in order to be able to diagnose diabetic retinopathy if necessary.
Complications
Diabetic retinopathy is associated with diabetes mellitus that has existed for many years and is associated with a wide variety of complications. The sugar, which has been increased over many years, chemically combines with proteins and larger molecules are formed that clog the smallest vessels and thus lead to the blood flow drying up. This leads to a reduced supply of blood to the eyes, for example (diabetic retinopathy).
The affected person notices that his eyesight is deteriorating, visual field defects are conceivable. Retinopathy can lead to blindness. This can mean impairments in everyday life, including road traffic. Furthermore, diabetes can also affect the kidneys (diabetic nephropathy), in the worst case it can lead to kidney failure.
Initially, there is an increased excretion of urine, which, however, becomes less and less in the course of the process. In addition, the blood becomes acidic, which leads to an increased concentration of potassium in the blood (hyperkalaemia). This can lead to cardiac arrhythmias, which can even end in cardiac arrest.
An impairment of nerve function (diabetic neuropathy) can also be explained by diabetes. This leads to disorders of sensitivity and paralysis. This makes it harder to identify wounds on the foot, as pain stimuli are no longer properly perceived. The wounds can enlarge over time and cause irreversible tissue damage (diabetic foot).
When should you go to the doctor?
Diabetic retinopathy is asymptomatic in the beginning and usually goes unnoticed for a long time. In order to be able to identify the first signs of an illness at an early stage, type 2 diabetics should undergo an ophthalmological examination immediately after the diagnosis. Annual check-ups are then recommended.
Type 1 diabetics are advised to visit their ophthalmologist for the first time no later than the fifth year after diagnosis of the diabetes or at the age of eleven; if the blood sugar level is poorly controlled, a much earlier examination is necessary. Pregnant diabetics are recommended to have an ophthalmologist checked every three months.
Basically, in the case of known diabetes mellitus, any deterioration in vision should lead to an examination by an ophthalmologist: Signs of this can be difficulty reading, the eyes quickly become tired or headaches caused by overwork. A visit to the ophthalmologist should be made immediately if visual disturbances such as blurred vision or dancing black dots occur.
If this "soot rain" occurs suddenly and is accompanied by a loss of visual field, acute bleeding or complete detachment of the retina must be assumed. Immediate ophthalmological treatment is essential in this case in order to maintain unrestricted vision. In addition to the ophthalmological check-ups, if you have a known diabetic retinopathy, your family doctor should regularly check the optimal setting of blood sugar, blood lipid levels and blood pressure.
Doctors & therapists in your area
Treatment & Therapy
Diabetic retinopathy can only be successfully treated if the underlying diabetes mellitus disease is consistently treated. Neither diabetic retinopathy nor diabetes mellitus can currently be definitively cured, but the vascular damage that has occurred in the retina can be improved or the progression of the disease prevented.
To avoid severe retinal damage, it is important to identify and treat diabetic retinopathy as early as possible. The patient must consistently implement the measures for diabetes treatment such as adequate nutrition as well as abstaining from cigarettes and excessive alcohol consumption.
Any hypertension that may be present also requires treatment. If new vessels have formed in the retina or if there is bleeding in the vitreous body in front of the retina, various laser therapies can be performed.
In the case of fluid retention at the yellow point (macular edema), an injection method is used in which drugs containing cortisone or drugs that inhibit vascular growth and cause the middle of the retina to swell are injected directly into the vitreous humor. The injection of cortisone preparations must, however, be repeated.
If retinal detachment has occurred or persistent bleeding into the vitreous humor is found, an operation is performed to remove the bleeding caused by diabetic retinopathy and reattach the retina.
Outlook & forecast
Diabetic retinopathy is not a curable disease. She has an unfavorable prognosis. Another complicating factor is that it is often only diagnosed at a very advanced stage. It is symptom-free for a long time and is therefore usually recognized late.
Drug treatment is unsuccessful with current medical options. The patient's behavior and good medical treatment are decisive for a better course of the disease. With an optimal adjustment of the blood sugar level, the progress of the disease can be influenced.
In some cases the diabetic retinopathy is no longer worsening. The eyesight remains at a continuous strength in these sufferers. For this, the patient has to get used to a diet that is adapted to their physical needs. This often requires a complete change in food intake.
This is to be observed until the rest of his life. Deviations lead to a deterioration in health and an increase in complaints within a short period of time. In addition to a special diet, the organism needs sufficient exercise. Obesity should be avoided and blood sugar levels should be checked regularly.
If the patient succeeds in adhering to the guidelines, there is a possibility that there will be no further decrease in vision. In some cases, laser therapy can also improve the visual system.
prevention
The best possible prophylaxis against diabetic retinopathy consists in recognizing diabetes mellitus and the diabetic retinopathy based on it as early as possible and in targeted treatment. The impending loss of vision can be avoided with early therapy.
Since diabetic retinopathy often does not cause any symptoms worth mentioning over long periods of time and thus remains inconspicuous, diabetics should consult an ophthalmologist once a year. Immediately perform an eye examination at the first sign of any deterioration in vision caused by diabetic retinopathy.
Aftercare
Diabetic retinopathy, a possible sequelae of diabetes mellitus, should be checked regularly by a qualified ophthalmologist in order to detect possible changes in the retina and thus prevent possible impairment of vision or, in the worst case, blindness.
With the help of fundoscopy, the ophthalmologist looks for small aneurysms or bleeding that can form in the vessels of the retina. If these are detected, it is possible to inform the patient about an operation in which certain areas of the retina are burned with the help of a laser. This prevents glaucoma (glaucoma), which can be caused by diabetes mellitus.
In addition, the patient should regularly check their blood sugar levels in order to check that the medication is being used correctly and thus to prevent further secondary diseases. In addition to the eyes, it is also important to check the kidneys, as kidney disease is also more common with the eyes. To do this, the patient should visit the nephrologist regularly.
Furthermore, the diabetic should have his or her foot checked by the family doctor, as a diabetic foot is not uncommon and can lead to amputation in the event of an acute deterioration in the condition. Neurological diseases should also be checked and treated by an appropriate specialist.
You can do that yourself
The main trigger factor in diabetic retinopathy is diabetes mellitus that has persisted for many years and in which the blood sugar was not optimally controlled. One of the most important preventive measures is therefore a strict self-control of blood sugar, which should not exceed certain values if possible. This applies to the by far most common type 2 diabetes as well as to the rare genetic autoimmune disease type 1 diabetes.
The adaptation and alignment of behavior in everyday life and the application of self-help measures have a great influence on the onset or avoidance of diabetic retinopathy. The retina is caused by damage in the blood vessel walls. This promotes the development of microaneurysms, so that after they burst, bleeding into the retina - in advanced stages even into the vitreous humor - occurs and causes corresponding visual impairments.
The most important self-help measures consist in the strict control and adjustment of blood sugar and blood pressure as well as in the diet change to an individually composed diet, which facilitates the control of the blood sugar level.
In addition, maintaining a normal weight and renouncing nicotine consumption as well as restricting alcohol consumption help to avoid retinopathy or to slow down or even stop the progression of the disease. Following the recommended self-help measures also favors the success of any medical therapies such as laser treatments on the retina.



.jpg)
.jpg)
.jpg)






.jpg)

.jpg)
.jpg)











.jpg)