A Glans inflammation becomes medical Balanitis called. It is a disease of the male limb that can also extend to the foreskin. Then the doctor speaks of one Balanoposthitis, so one Foreskin inflammation.
What is glans inflammation (foreskin inflammation)?
.jpg)
© joshya - stock.adobe.com
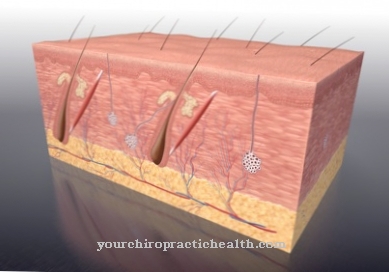
Glans inflammation is an inflammatory skin disease of the glans on the penis. The foreskin is also often affected. Sometimes there are purulent secretions around the swollen glans.
The causes can be different, they also depend on the age of the person affected. Inflammation of the glans can become chronic. Then the foreskin hardens, resulting in a narrowing of the foreskin, which can also be chronic.
Glans inflammation can occur in both young and adult men.
causes
Depending on age, the causes of glans inflammation or foreskin inflammation can be very different.
In pre-puberty boys, about one in every 20 boys has glans. Here you will often find constrictions or adhesions of the foreskin. The inflammation is often infectious.
In younger, sexually mature men, glans inflammation is less common than in children, and sexual activity is often the cause. Glans inflammation can be both infectious and non-infectious.
In older men, balanitis is rarely infectious. The cause of this is often the lack of personal hygiene. In very elderly men, thinning skin and tissue softening can lead to glans inflammation.
Finally, glans also occur as a result of other diseases. Diabetics, for example, have an increased risk of an infectious glans inflammation. After all, contact with women who suffer from vaginal thrush also often leads to balanitis.
Symptoms, ailments & signs
Glans inflammation manifests itself primarily through the noticeable reddening of the glans skin. Often the inner sheet of the foreskin is also reddened. The affected areas of the skin can ooze and flake off. Usually itching, burning and increased sensitivity to touch are added.
In individual cases, ulcers form in the area of the foreskin, which are associated with severe pain and an increased risk of inflammation. Other symptoms depend on the form of the glans inflammation. The balanitis simplex is noticeable through blurred reddening with nodules and dry flaking. Most of the time, the skin changes appear suddenly and change within a short time.
This form can occur in men of any age group. This is not the case with balanitis plasmacellularis, which usually develops from the age of 60. In this form, there are several sharply defined rednesses that can be recognized by their unusual shape.
They are usually weeping, shiny, varnish-like and in some cases develop into superficial skin defects that are particularly sensitive to pressure and other external stimuli. Fine, punctiform hemorrhages can be noticed within the spots. The Balantatis plasmacellularis typically takes a chronic course and can remain unchanged for months or years.
Diagnosis & course
The doctor determines an inflammation of the glans on the basis of microbiological examinations. To do this, he examines the patient's urine and smears the glans. Of course, the diagnosis also includes questioning the patient.
Since glans glans can have various causes, the doctor must first determine them, because only then is an effective therapy possible. The glans inflammation manifests itself in a reddening and swelling of the glans. The patient has a burning sensation on the glans penis and complains of itching.
Oozing, watery or purulent secretions may occur. Blistering is also possible.
If the inflammation continues and is untreated, a fever may occur. Pain when urinating is also possible.
The glans inflammation can spread through the urethra to the kidneys and lead to bladder, urinary tract and prostate infections. Finally, sepsis can also occur.
When should you go to the doctor?
In the case of itching, burning, and redness on the glans, glans may be the cause. A visit to a doctor is recommended if the symptoms do not go away on their own after a week at the latest or if further symptoms appear.
In particular, ulcers and weeping skin defects must be clarified immediately. Likewise, discharge and whitish deposits on the glans. If there are adhesions, the skin disease lichen sclerosus may be the cause - an immediate doctor's visit is advisable in order to avoid the impending narrowing of the foreskin.
Patients who have been infected with herpes viruses, chlamydia, fungi or parasites in the past are particularly prone to glans. People with a contact allergy, allergies or existing autoimmune skin diseases (e.g. psoriasis, nodules, diabetes mellitus or HIV) are at risk and should consult a doctor as soon as possible if the symptoms are mentioned.
At the latest when complications arise and, for example, epididymitis develops, a doctor must be spoken to. Otherwise, the inflammation can spread and in the worst case cause blood poisoning.
Doctors & therapists in your area
Treatment & Therapy
If acorn inflammation is treated consistently, it has a positive course and usually heals without complications. The goal is to treat the symptoms and inflammation.
The treatment is first of all a local therapy. As soon as the pathogen is determined by the smear and / or the urine test, treatment is carried out with an appropriate ointment containing antibiotics or with a cream that kills fungi.
If the balanitis is not caused by an infection, the inflammation can be treated with an ointment containing cortisone. Chamomile baths can be useful to relieve itching.
If the glans infection becomes chronic, the patient should consider circumcision. However, circumcision is contraindicated in boys under three years of age, as circumcision appears to significantly increase the risk of inflammation up to this age.
Treatment of adult patients also requires that the patient's sexual partner also be examined.
Finally, if the findings are unclear, the doctor should also take tissue samples for differential diagnosis and submit them for histological examination in order to identify a possible precancerous stage at an early stage.
Outlook & forecast
If treated, an inflammation of the glans has a very good prognosis. The duration and level of suffering of the disease depend on the cause of the inflammation and the immune system of the person affected. If bacteria or fungi are decisive, appropriate medication can provide relief within days or weeks.
The damaged tissue of the glans penis and foreskin can be treated well with anti-inflammatory ointments and soothing baths. In the rarest of cases, permanent tissue damage is to be feared. Occasionally less sensitive areas develop and an acquired phimosis due to an infection of the foreskin and glans penis. If the inflammation has another cause, for example insufficient hygiene or an injury to the glans penis or foreskin, good results can also be achieved with protection and ointments.
An untreated glans inflammation with a bacterial trigger, on the other hand, harbors the risk that the infection will spread further. It can reach the bladder, prostate and kidneys and in the worst case lead to sepsis. This can be fatal if left untreated. However, this can only occur if a bacterial infection on the penis remains untreated for a long time.
Fungal infections carry a similar risk of spreading. In very rare cases, ulcers and cancer precursors develop due to balanitis. If there is no medical intervention here, there is a risk of cancer breaking out and permanent loss of tissue on the limb. Overall, circumcision lowers the risk of developing another balanitis.
prevention
First of all, proper personal hygiene is important in preventing acornitis. However, proper genital hygiene does not mean that cleaning the foreskin should be overdone.
Normal but regular washing of the glans without soap and shampoo, with pulling back the foreskin and removing the smegma, should be part of a man's normal personal hygiene.
Chamomile baths and rinses with saline solutions are also part of the prevention of acorn inflammation.
Condoms during intercourse also reduce the risk of glans inflammation. A condom should be an absolute must during sexual intercourse in order not to infect the intimate partner, especially if an illness has developed.
You can do that yourself
Balanitis should be treated by a specialist doctor. Once the pathogen has been identified, specific treatment can be carried out using an antibiotic or antifungal ointment. If a foreskin constriction is the cause of recurring inflammation, those affected or the parents of affected children should find out about a surgical procedure.
Chamomile baths or brine baths are recommended. The penis can then be dabbed with olive oil. This cares for the inflamed foreskin. After every urination, the penis should also be cleaned with water so that no urine residues remain on the foreskin. Furthermore, those affected can check whether an allergy to certain substances - such as latex in condoms - is responsible for the inflammation and should avoid this in the future.
Naturopathy recommends alkaline baths to balance the acid-base balance as well as the support of the intestinal flora with probiotics, since inflammation is always associated with a weakened immune system. The remedies: Arnica (decongestant), Calcium floratum (has a strengthening effect), Hepar sulfuris (diverting) and Tuja (skin diseases) can have a supportive effect.
Thorough intimate hygiene is also important after the symptoms have subsided. Regular cleaning of the penis with water - soap and shampoo should be avoided - is sufficient. In the case of recurring infections, the sexual partner should also have an examination carried out in order to rule out that pathogens are repeatedly transmitted through sexual intercourse. The use of condoms is recommended as a preventive measure, especially if there are changing intimate partners.

.jpg)

.jpg)
.jpg)






.jpg)
.jpg)
.jpg)







.jpg)