fibrin is a water-insoluble, high-molecular protein that is produced from fibrinogen (coagulation factor I) during blood clotting by the enzymatic action of thrombin. The medical specialties are histology and biochemistry.
What is fibrin?
During blood clotting, fibrin is formed from fibrinogen under the action of thrombin. Soluble fibrin is formed, also called fibrin monomers, which polymerizes to a fibrin network by means of calcium ions and factor XIII. Fibrin molecules obstruct blood flow in a pathological process. Fibrinolysin dissolves the resulting blood clots.
Fibrin is a protein and an important endogenous substance that is responsible for blood clotting. It is caused by the action of the clotting enzymes prothrombin and fibrinogen, which are produced in the liver. Fibrin consists of fiber-like molecules that network with one another through a fine lattice. Fibrin grids are an indispensable prerequisite for blood clotting. Medical terminology also uses the terms plasma fiber, blood fiber and globular plasma protein (serum proteins, blood proteins).
Anatomy & structure
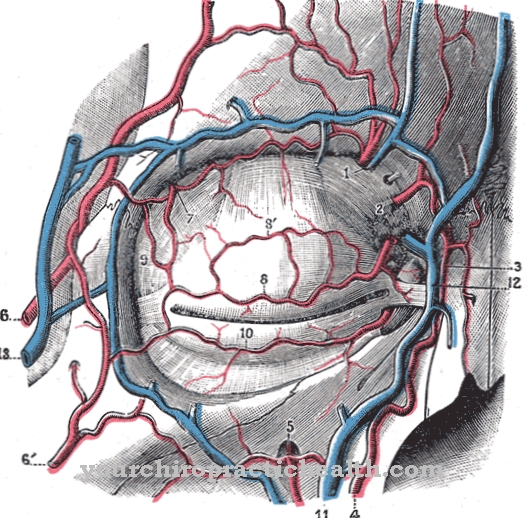
There is no finished fibrin in the blood, only the soluble precursor fibrinogen. Usually, the solid and liquid components of the blood do not separate easily. When the blood leaves the body, long fibrin fibers are created that spin the blood cells into a clump in the form of a blood cake. This process is indispensable for properly functioning blood clotting.
The emerging blood platelets stick to the fibrin fibers of the wound edges. After about three minutes of bleeding, enough platelets are attached to each other at the injury site to form a clot that stops the bleeding. The wound plug is given the necessary strength through the network of fibrin threads that are created. Fibrin causes blood coagulation through its ability to cross-link polymerisation (reaction processes that lead to the formation of molecular substances). Fibrin is one of the blood clotting factors. These substances are the cause of blood clotting after injuries and ensure that bleeding is stopped. There are different blood coagulation factors, which are designated with the numbers I to XIII. Fibrinogen is the most important coagulation factor I.
Blood clotting in the body takes place in a cascade. To stop bleeding and help blood to clot, fibrinogen is converted into fibrin. This forms chain-like structures that stabilize the clotting plug. The fibrinogen forms the non-crosslinked precursor of fibrin. After an injury during blood clotting, two small peptides (fibrinopeptides) are split off under the action of the serine protease thrombin, which convert it into monomeric fibrin. The polymer fibrin is then formed from this covalent cross-linking with the participation of calcium (calcium ions) and blood coagulation (factor XIII). The result is a fibrin scaffold with which platelets, erythrocytes and leukocytes stick together and lead to the formation of thrombus.
Plasmin enables the subsequent breakdown of the fibrin (fibrinolysis). Fibrinogen is one of the acute phase proteins that can indicate inflammation in the body. The human body has thirteen coagulation factors: factor I fibrinogen, factor II prothrombin, factor III tissue thrombokinase, factor IV calcium, factor V proaccelerin, factor VI corresponds to activated factor V, factor VII proconvertin, factor VIII hemophilia - A factor, is absent Hemophilia, factor IX hemophilia - B factor, factor X Stuard power factor, factor XI Rosenthal factor, factor XII Hagemann factor, factor XIII fibrin-stabilizing factor. This classification is not identical to the sequence of activation in blood clotting.
The reaction steps take place in different ways, depending on the injury. The coagulation factors are designed in such a way that, when activated, they go through precisely coordinated steps for fibrin production in a chain reaction.
Function & tasks
The coagulation system protects the organism from bleeding to death by quickly stopping bleeding in smaller vessels. The body's own protein plasma fiber helps in this process and acts like an adhesive. A normally intact vascular system is not only at risk in the case of injuries caused by external influences and which are immediately noticeable.
The smallest vessels in the human body are regularly injured or leaky, for example through impacts or inflammation. The arterial system is constantly under pressure. For this reason, even the smallest vascular injuries are suitable for causing bleeding out of the vessel. To prevent this process, the coagulation system seals these leaky vessels from the inside. The coagulation mechanism runs in several stages by controlling the blood plasma substances in the form of coagulation factors (I to XIII). Three reaction sequences form a chain reaction. The vascular reaction limits blood loss by narrowing the affected blood vessel.
The platelet plug brings about hemostasis by briefly occluding the blood vessels. Long-term vascular occlusion occurs through the formation of a fiber network made of fibrin. In the liver, the coagulation proteins prothrombin are formed as a precursor of thrombin and fibrinogen as a precursor of fibrin. These two substances end up in the blood plasma. The blood plasma is transformed into prothrombin with the help of the enzymes blood thrombokinase, tissue thrombokinase and calcium ions. This becomes thrombin and fibrinogen becomes fibrin. Fibrin forms the tissue network that is indispensable for hemostasis and stops the bleeding.
Diseases
If the human coagulation system no longer works properly, severe disorders occur that significantly restrict blood circulation. Depending on the underlying disorder, excessive blood thickening can lead to the formation of blood clots such as thrombosis and embolism. Excessive blood thinning causes an increased tendency to bleed or life-threatening bleeding.
The cause can be both hereditary and platelet disorders or clotting factors. Occasionally, coagulation problems also appear as a symptom of other ailments or diseases that are independent of the coagulation system, such as an injury. Fibrinogen is determined if various diseases are suspected, if the patient has an excessive tendency to bleed (haemorrhagic diathesis) or a tendency to form blood clots (thrombosis).
In addition, the fibrin is determined during treatment with streptokinase (extracellular protein, antigen) or urokinase (plasminogen activator, enzyme of the peptidases) to dissolve a blood clot (fibrinolysis therapy) for monitoring purposes and in the event of abnormal activation of blood clotting (consumption coagulopathy). The value is determined from the blood plasma.




















.jpg)



