Listeria Commonly found in raw foods like ground beef, raw milk, fish, and salads. These are extremely adaptable bacteria that can be found all over the world and hardly need any nutrients to survive. How resistant these bacteria are is shown by the fact that they can survive even in the absence of air in a vacuum, as well as at refrigerator and freezer temperatures. Only sufficient heating of at least 70 degrees Celsius kills Listeria.
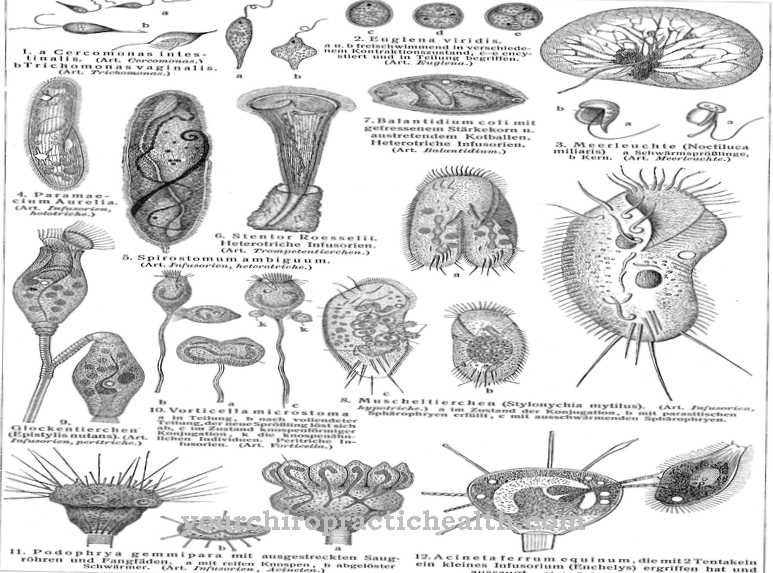
What are Listeria?
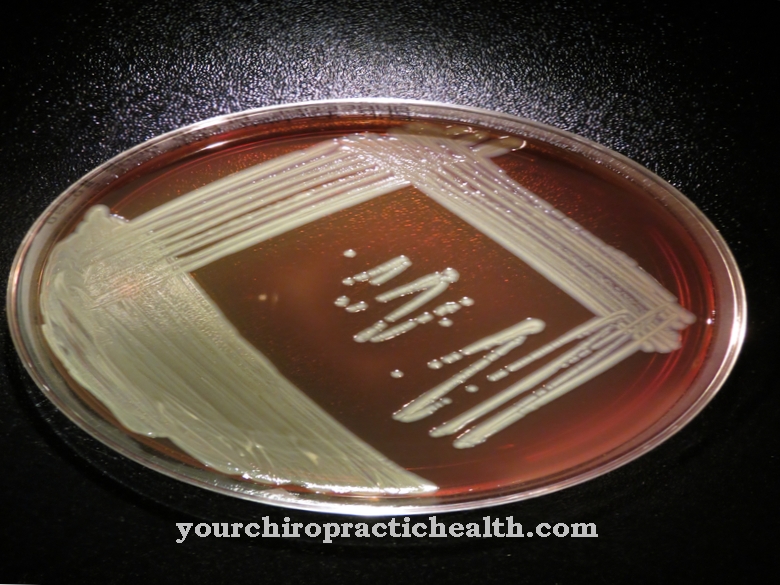
Listeria are undemanding bacteria that can survive under almost all environmental conditions. They are gram-positive, anaerobic and endospore-forming bacteria. The 1.5 µm rod-shaped and thread-like bacteria move actively by swimming. They are ubiquitous in nature, because the resistant bacteria can multiply even in nutrient-poor substrates such as condensation and puddles. The extremely cold and heat tolerant Listeria die only at a temperature of 70 degrees Celsius and are often found in raw meat and raw milk products.
There are different types of dangerous Listeria. The most common species is Listeria monocytogenes. The Federal Institute for Consumer Health Protection and Veterinary Medicine recommends a limit value of 100 germs per milliliter or gram of food, as there is no legally prescribed limit value in Germany. The minimum infectious dose (MID) at which Listeria trigger a disease is still unknown. However, medical professionals assume that there must be a very high concentration of bacteria.
Occurrence, Distribution & Properties
Since Listeria are very undemanding and resilient, they can be found almost everywhere in nature. They are heat and cold tolerant and can survive even in the most adverse environmental conditions. Since the 1.5 µm rod-shaped and thread-like bacteria can swim, they are often found in running water, in puddles and condensation. You will also feel comfortable on plant materials such as dead grass and in the intestinal tract of animals and humans.
About ten percent of people are carriers of Listeria and excrete them through the stool. People come into contact with Listeria through contaminated food, which is mainly found in raw meat products, fish and raw milk products. Since listeria are ubiquitous in the environment, they can also be found on plant foods such as lettuce.
In contrast to their natural occurrence in nature, Listeria only find its way into the aforementioned foods in a roundabout way, because the contamination occurs in the different stages of production during food processing due to poor hygiene and insufficient heating.
By fertilizing with animal waste water such as liquid manure, Listeria can get on vegetables and salads. These bacteria also survive in vacuum-packed foods because they are able to switch between aerobic and anaerobic metabolism. This ability means that, unlike many other germs, Listeria can survive even when there is less oxygen.
These bacteria record optimal growth rates in a temperature range between 30 and 37 degrees Celsius with a pH value between 5.0 and 9.0 and a slightly increased carbon dioxide concentration. Even under extended temperature conditions, Listeria can survive when competing germs have long ceased their activity. However, frying, boiling, pasteurizing and sterilizing kill the germs. In sour or salty pickled foods, reproduction is only delayed or no longer possible.
Infection cannot always be reliably prevented, because Listeria infection is possible almost everywhere. These bacteria arise not only during the production and processing of food by the manufacturers, but also through improper storage and preparation in the home kitchen. Due to technical errors in the kitchen such as contaminated knives, cutting machines, documents, plates and improper storage and preparation conditions, listeria can spread ubiquitously and lead to so-called listeriosis. Washing your hands before and after preparing food also helps prevent infection.
There is also an increased risk of Listeria in factory farming, because these unfavorable housing conditions produce an increased infection potential of the livestock. People who are particularly at risk from a listeria infection should refrain from consuming foods from the high-risk group.
Illnesses & ailments
Listeria are usually harmless to people with a healthy immune system because they are excreted in the bowel with the bowel movement. It is estimated that 10 percent of people are infected with Listeria without it becoming noticeable as long as the immune system is functioning properly.
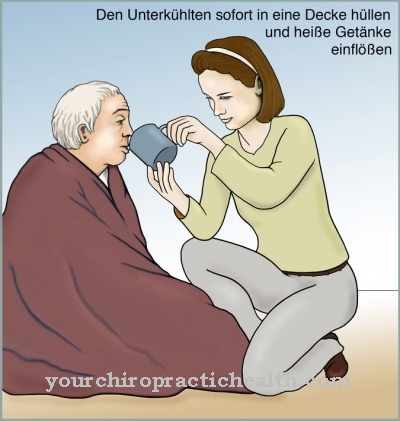
The bacteria are dangerous for people with a weakened immune system, which is caused, for example, by tumor or flu diseases, HIV or an organ transplant. Elderly people, infants, toddlers and pregnant women also belong to another risk group.
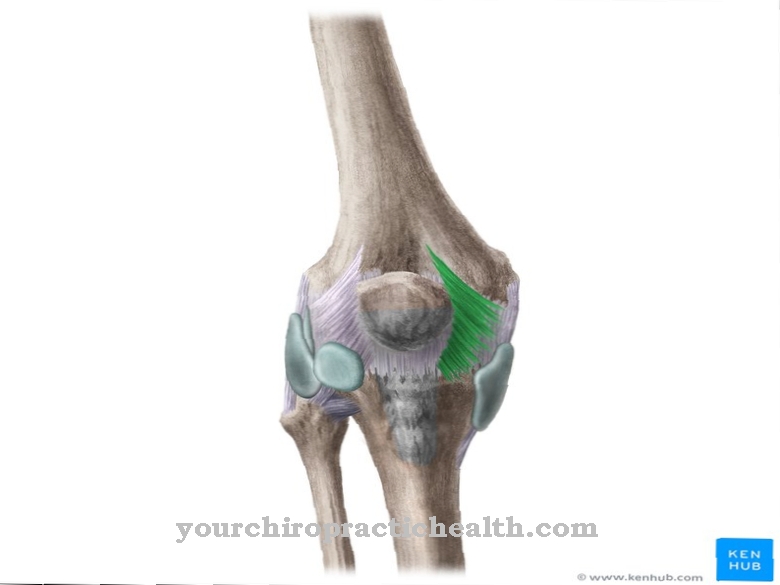
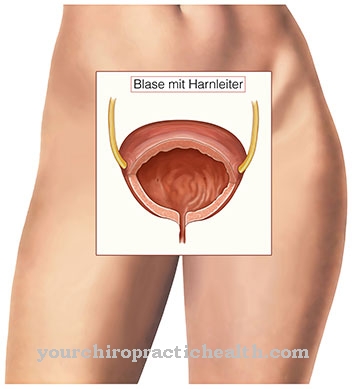
Listeriosis manifests itself with flu-like symptoms such as fever, muscle pain, vomiting, and diarrhea. Often these symptoms are accompanied by purulent inflammation of various organs, with meningitis (meningitis) and blood poisoning (sepsis) occurring the most frequently. Inflammation of the brain (encephalitis), the conjunctiva (conjunctivitis), the joints (arthritis) and the heart valves (endocarditis) are less common.
If there is a suspicion of listeriosis, the diagnosis is made using body fluids such as blood, nerve water, weekly fluids or suspicious foods. The examination of a stool sample, on the other hand, is not expedient, since many people carry Listeria without becoming ill.
The treatment is carried out with high-dose antibiotics such as amoxicillin and gentamicin. If the healing is not successful, co-trimoxazole is administered. Other treatment options include macrolides, chloramphenicol, and vancomycin. The treatment time depends on the severity of the disease and lasts two to six weeks.
A detailed guide is available from the Institute for Risk Assessment, which covers all the important questions relating to the subject of food infections and gives tips on how to prevent them.






.jpg)


.jpg)


.jpg)




.jpg)