Hemostasis is a term for hemostasis. After an injury to a vessel, various physiological processes take place that bring the bleeding to a standstill.
What is Hemostasis?

As part of hemostasis, the body stops bleeding caused by injuries to the blood vessels. This prevents large amounts of blood from escaping.
Hemostasis can be divided into two processes. However, both are closely related and interact with one another. Primary hemostasis is responsible for stopping the bleeding after about one to three minutes. It is in turn divided into the three steps of vasoconstriction, platelet adhesion, and platelet aggregation. Primary hemostasis is followed by secondary hemostasis, which lasts about six to ten minutes. Here, too, a distinction is made between three different phases (activation phase, coagulation phase and retraction phase).
Disturbances in hemostasis can manifest themselves as a tendency to bleeding or inadequate hemostasis.
Function & task
Primary hemostasis is the hemostasis phase. Immediately after the injury, the injured vessels contract. This process is known as vasoconstriction. The vasoconstriction results in a narrowed vessel lumen prior to the injury. This causes the blood flow to slow down in the injured area.
Blood platelets (thrombocytes) attach to certain components of the injured vessel walls. The glycoprotein receptor Ib and / or the glycoprotein receptor Ic / IIA are required for this adhesion reaction. The adhesion of the platelets leads to an initial provisional covering of the wound. These mechanisms stop the bleeding after one to three minutes.
Secondary hemostasis is the actual blood clotting phase. The temporary closure is replaced by a more stable fibrin mesh in three steps. When platelets come into contact with external factors, various coagulation factors are activated.
Negatively charged surfaces can be found, for example, on glass or stainless steel. The activated coagulation factors set a coagulation cascade in motion. If the coagulation cascade is started in this way, an activation of the intrinsic system is the basis. The extrinsic coagulation system is activated by the contact of blood with injured tissue. Here, too, a coagulation cascade follows.
At the end of the coagulation cascade there is enzymatically active thrombin in both the intrinsic and the extrinsic system. This causes the fibrin to polymerize. Fibrin is created from the inactive fibrinogen. The so-called factor XIII ensures that the individual fibrin threads connect with one another. This stabilizes the platelet plug that has formed in the primary phase and solidifies the wound closure. The resulting plug is called a red thrombus.
The thrombin also causes the actin-myosin skeleton of the platelets to contract. The platelets contract, pulling the edges of the wound together. This closes the wound. The contraction of the wound and the platelet-derived growth factor (PDGF) promote the immigration of connective tissue cells. From this point on, wound healing begins.
In summary, hemostasis is a vital process that stops bleeding in the event of an injury. This will prevent the excessive loss of blood. At the same time, the prerequisites for rapid healing of the wound are created.
Illnesses & ailments
Disturbances in hemostasis can lead to inadequate and excessive hemostasis or blood clotting. The causes of these defects lie at the level of fibrinolysis, platelets or the actual coagulation.
Diseases which are associated with an increased tendency to bleed fall under the term "hemorrhagic diathesis". The hemorrhagic diatheses can be divided into four groups according to their pathomechanisms: thrombocytopathies, thrombocytopenias, coagulopathies and vascular hemorrhagic diatheses. Hemorrhagic diatheses include diseases such as hemophilia A, hemophilia B, Osler's disease, Henoch-Schönlein purpura, hypersplenism, consumption coagulopathy or Willebrand-Jürgens syndrome.
All these diseases are characterized by an increased tendency to bleed. The bleeding is either too long, too heavy or is caused by the smallest of injuries. In the hemophilic bleeding type, the bleeding is very extensive and relatively sharply defined. Bleeding into joints or muscles is typical here. Large-scale bruises appear after banal injuries. This bleeding occurs in diseases such as hemophilia A or hemophilia B.
In thrombocytopenia or in vascular diathesis, the bleeding occurs in the form of petechiae or purpura. Petechiae are small punctiform hemorrhages in the skin or mucous membranes. With purpura there is multiple, small-patch bleeding in the skin.
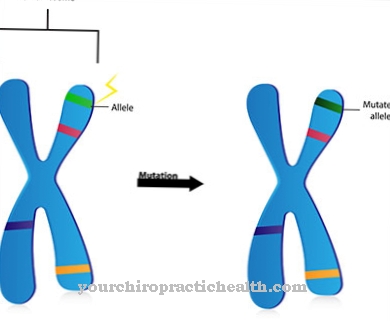
Diseases that are associated with excessive hemostasis are referred to as thrombophilia. There is an increased tendency to thrombosis here. Hypercoagulability can be demonstrated in the laboratory. Thrombophilias can be congenital or acquired. Acquired risk factors for developing thrombophilia are obesity, smoking, pregnancy, estrogen-based contraceptives, heart failure and immobility after surgery or a long illness.
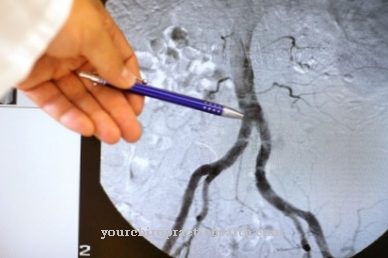
Genetic risk factors include antithrombin deficiency, protein C deficiency, or protein S deficiency. In hemophilia, blood clots can form in all of the blood vessels in the body. However, preferred locations are the deep leg veins. The thromboses often go unnoticed. Even severe thromboses that later lead to pulmonary embolism are often asymptomatic. With pronounced venous thrombosis, the ankles, the lower leg or the entire leg swell. The affected extremity is also warm. The skin is tense. The feeling of tension and pain can also occur throughout the leg. The most dangerous complication of thrombosis is pulmonary embolism. Here the thrombus migrates from the leg into the arteries of the lungs, where it causes a life-threatening vascular occlusion.








.jpg)





.jpg)