The Haglund syndrome, also as Haglund heel is caused by a bony change (overbone) on the heel bone in the area of the Achilles tendon attachment. The name goes back to the Swedish surgeon Patrik Haglund (1870-1937). Haglund's heel can be extremely painful and can be treated conservatively or surgically.
What is Haglund Syndrome?
.jpg)
© blueringmedia - stock.adobe.com
The Haglund heel, a type of heel spur, can be recognized by a bony change in the upper rear (cranial and dorsal) part of the heel bone (calcaneus) in the area of the Achilles tendon attachment.
Ossification on the heel bone can already occur during the growth phase at the growth plate of the bone (epihyseal plate) or it can be ossification on the heel bone directly in the area of the Achilles tendon attachment (apophysis). Such bone expansions with solid bone substance on the heel bone are also known as "Haglund exostosis".
Disturbances in the growth plate occur exclusively in adolescents because the growth plate closes after the bone growth is complete due to regular ossification. Such disorders in the growth plate of bones are called "iuvenile osteochondroses". Both forms of Haglund's syndrome can trigger similar symptoms and cannot be precisely differentiated from one another.
causes
The main causes of Haglund heel formation are seen in footwear, which irritates the tendons or puts direct pressure on one or more of the bones in the foot. For the bone, this can be an incentive to increase bone formation in the affected area.
Shoes with tight heel counters can cause constant irritation to the Achilles tendon insertion when walking and running and mark the beginning of the formation of a Haglund heel. Excessive running training with inadequate footwear and being overweight are also cited as contributing factors for causing Haglund syndrome.
The extent to which genetic dispositions can lead to premature and excessive ossification of the growth plate of the calcaneus has not yet been conclusively clarified. Here too, inadequate and tight footwear in children is the main culprit. Congenital or acquired foot deformities can also promote the development of a Haglund heel.
Symptoms, ailments & signs
Haglund's syndrome is primarily noticeable through sharp pain in the back of the heel bone. The pain occurs with load and pressure on the heel and quickly subsides again as soon as the leg is relieved. The pain is very intense at first and recedes with repeated stress. The pain is strongest in the morning and after a long period of rest.
Outwardly, the Haglund Syndron can be recognized by the striking gait. Those affected usually limp or drag their leg with the affected heel. Sometimes the heel will become red or have a visible swelling that is painful to the touch. In individual cases a visible ossification can be noticed on the heels or on the upper posterior tendon attachment of the heel.
These ossifications are painful to the touch and are occasionally associated with swelling and redness. If Haglund syndrome is left untreated, it becomes more intense. The avoidance behavior can result in misalignments and joint wear. Some people also suffer from nerve pain that can radiate from the heel to the knee. In individual cases, the Haglund heel causes symptoms of paralysis and sensitivity disorders, which those affected find uncomfortable.
Diagnosis & course
The first symptoms that indicate a Haglund heel are externally recognizable redness, pressure-sensitive areas or even thickening on the upper rear part of the heel bone.
If orthopedic examinations confirm the initial suspicion of Haglund's syndrome, diagnostic imaging methods such as ultrasound, X-rays and computed tomography (CT, MRI, fMRI) can provide more precise information. In the X-ray image, bony formations in particular are clearly visible. The computed tomography processes also provide meaningful images of the soft tissues, i.e. the nature of ligaments, tendons, muscles, bursa and articular cartilage.
The course of the disease in a Haglund heel are very different and range from completely painless to very painful and debilitating. The symptoms of the disease can develop over a long period of time, so that emerging symptoms - especially when there is no pain and no serious impairment associated with it - are ignored and not treated.
Complications
Haglund's syndrome primarily results in relatively severe pain. This pain has a negative effect on the patient's everyday life and can therefore significantly reduce the quality of life and lead to restricted mobility. It is not uncommon for Haglund Syndrome to lead to pain at rest and thus to sleep disorders in the patient. The skin is reddened by the disease and ossification occurs, which mainly occurs on the patient's heels.
The pain can also spread to other regions of the body. Due to the restricted mobility, the patients often suffer from depression and other mental disorders. In some cases, patients are also dependent on walking aids in order to cope with everyday life. There are no further complications with the treatment itself.
Most complaints can be limited by wearing suitable footwear. In many cases, however, physiotherapy is still necessary. If there is no improvement, surgical interventions are usually necessary. Life expectancy is not affected by Haglund syndrome.
When should you go to the doctor?
Since Haglund syndrome does not heal itself and the syndrome is usually associated with severe pain and restrictions in everyday life, medical treatment must always take place. Those affected should then consult a doctor if the skin becomes red. This redness usually occurs without a specific reason and in different parts of the body. In addition, there is ossification on the heel, which occurs especially at a young age.
This is noticeable through pain, which can occur not only as pressure pain, but also as pain at rest.If the child complains of pain in the heel, a doctor should definitely be consulted. Usually, Haglund syndrome can be diagnosed by a pediatrician or a general practitioner. However, the support of a specialist is necessary for further treatment. Early diagnosis increases the chances of a complete cure for Haglund syndrome.
Doctors & therapists in your area
Treatment & Therapy
If a diagnosed Haglund syndrome can essentially be traced back to unsuitable footwear, the first measure is to relieve the heel area. In addition, special physiotherapy is recommended, which aims to strengthen the leg muscles and relieve the Achilles tendon.
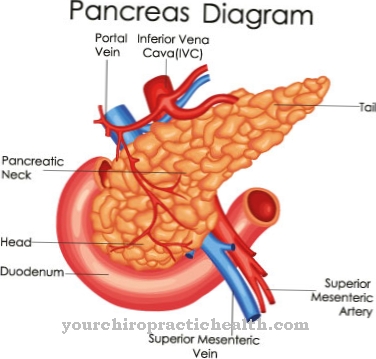
The use of extracorporeal shock wave therapy, which was originally developed for breaking up kidney stones, is also worth considering. Using shock wave therapy, limescale deposits and hardening in the tissue can be "pulverized" in such a way that they can be removed from the body via lymph and blood vessels and flushed out.
If conservative forms of therapy do not lead to the desired success, two different surgical interventions can be considered. On the one hand, the ossification can be removed directly in a surgical procedure. However, this has the disadvantage that the tendon sheath must also be removed in the area of the Achilles tendon attachment, which normally ensures problem-free gliding of the tendon. There is a risk that adhesions will develop on the tendon postoperatively, which can impair its function.
On the other hand, a surgical procedure has become established that does not touch the area of the Achilles tendon, but separates a wedge from the heel bone a few centimeters further forward so that the heel bone folds up a little in the area of the Achilles tendon attachment. The spur process is not removed, but if successful, it no longer presses or rubs the Achilles heel, so that the symptoms improve or even disappear completely.
Outlook & forecast
The prognosis for Haglund syndrome is usually very good with treatment. However, it is a very time-consuming therapy that is initially started with conservative measures. Without treatment or after constant exposure to the wrong footwear, athletic stress on the foot or being overweight, the symptoms can worsen considerably. The bone protrusion (haglund exostosis) on the heel bone will increase under these conditions because the pressure on the inner edge of the shoe increases when you run or walk.
Conservative treatment begins with the provision of orthopedic shoes. With their help, the mechanical stress on the bursa is supposed to be reduced and the inflammatory processes stopped. This treatment also includes the topical application of anti-inflammatory drugs and the injection of corticosteroids into the Achilles tendon. The therapy should show first results after approx. 6 months.
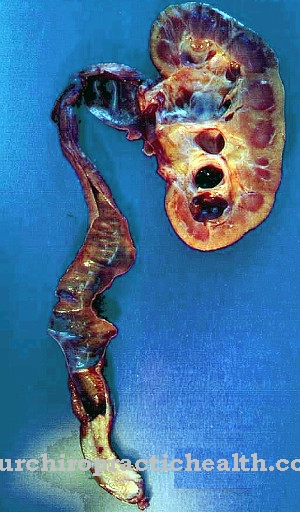
If the treatment is unsuccessful, however, an operation will be necessary. Usually the bursa (bursa subachillea) and the adjacent bony protrusion are removed. However, this operation must not be performed on children and adolescents up to the age of 17 because the neighboring growth plates are not yet closed.
After surgical removal or reduction of the protruding bone, the pressure of the inner edge of the shoe against the heel bone is reduced. This also reduces the pressure on the bursa, Achilles tendon and soft tissues. This treatment method usually leads to lasting success.
prevention
One of the most important things you can do to prevent the Haglund heel is to make sure you have suitable and functional footwear. Particularly in children whose feet are subject to certain growth spurts, attention should be paid to suitable footwear that gives the foot enough space for their development.
Other preventive measures are to carry out athletic running training exclusively with running shoes and to plan for enough stretching exercises. Consultation with an orthopedic specialist is recommended at the first signs of Haglund's syndrome.
Aftercare
With Haglund syndrome, the person affected has either very few or no direct follow-up measures available. First and foremost, the disease must be recognized quickly and, above all, at an early stage so that there are no further damage or complications to the feet. The person affected should consult a doctor and initiate treatment at the first symptoms or symptoms of the disease.
The treatment is usually carried out by surgery. The person affected should definitely take it easy and rest after such an operation. You should refrain from exertion or physical activity in order not to unnecessarily burden the body. The help and support of one's own family and friends can also have a positive effect on the patient's recovery.
Physiotherapy is usually necessary after the procedure. Many exercises from such a therapy can also be performed in your own home in order to accelerate the treatment. Regular examinations by a doctor are also very useful. Haglund syndrome usually does not have a negative effect on the life expectancy of the patient.
You can do that yourself
With Haglund syndrome, the possibilities for self-help are severely limited. In particular, an early diagnosis can prevent further complications and complaints. However, if Haglund syndrome has already occurred, only therapy or surgery can alleviate the symptoms.
However, the syndrome can be avoided simply by always wearing suitable footwear for children. This is especially true during the growth spurts. The feet must not be crushed and must have enough free space. Furthermore, sporting activities should always be carried out in running shoes or sports shoes. This can also prevent the syndrome.
If the syndrome occurs, unnecessary stress on the feet must be avoided in any case. At the first signs of the disease, an orthopedic surgeon should be consulted immediately, who can diagnose and treat the disease.
Children should always be informed about the possible complications and risks of Haglund syndrome in order to avoid open questions and possible psychological complaints. As a rule, the disease can be treated relatively well with surgery, so that there are no further restrictions in the child's development.


.jpg)
.jpg)






.jpg)
.jpg)


.jpg)