The Stroke volume will also be Stroke volume (SV) called. It tells you how much blood is expelled from the left ventricle of the heart during systole.
What is the stroke volume?

The term stroke volume comes from medicine. The heartbeat volume is called in English Stroke volume designated. It refers to the volume of blood that is ejected from the heart in a single heartbeat.
Usually the stroke volume is 70 to 100 milliliters. The stroke volume is the same in both heart chambers. Decreased stroke volumes can be found, for example, in heart attacks or in heart valve defects.
Function & task
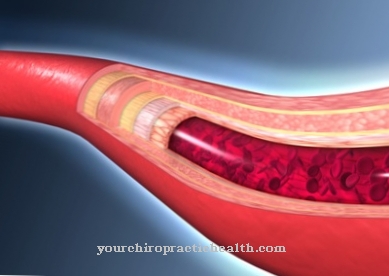
The heart is a pressure and suction pump that pumps around five to six liters of blood through the body every minute. From an anatomical point of view, the heart consists of two chambers and two atria. The atria are also known as the artria and the ventricles are called the ventricles. The atria and ventricles are separated from one another by the heart septum and the heart valves.
The venous blood from the body's circulation reaches the right atrium of the heart. From there it is pumped in diastole through the tricuspid clamp into the right ventricle. The blood then passes through the pulmonary valve into the pulmonary arteries and finally into the lungs. The gas exchange takes place there. The blood flows from the small pulmonary vessels via the pulmonary veins into the left atrium. During diastole, blood flows through the mitral valve into the left ventricle and, during systole, is ejected into the great arterial circulation.
The main task of the heart is to maintain the circulation. The heart also plays an important role in regulating blood pressure. But the heart can not only regulate blood pressure with the help of the heartbeat volume, it also reacts to various changes with a changed heartbeat volume.
One mechanism that regulates the amount of ejection is the Frank Starling Mechanism. Thanks to this mechanism, the heart's activity can be adapted to fluctuations in pressure and volume. The goal is that both heart chambers, i.e. both the left and the right heart chamber, always produce the same heartbeat volume.
Central terms in the Frank Starling mechanism are the preload and the afterload. The preload describes the filling of the atria. It is also called the preload. With an increasing preload, the chamber filling also increases. The heart rate stays the same, but the chambers expel more blood. If the venous return flow of the blood is reduced, the stroke volume is also automatically reduced.
Even if there is an increase in the arterial vessels, the stroke volume is regulated via the Frank Starling mechanism. If the resistance in the blood vessels increases, one speaks of an increased afterload. So that the heart can pump against the increased pressure, a higher pressure must be generated in the systole during ejection. The stroke volume decreases due to the increased force of contraction. This increases the preload in a next step. In this way, the stroke volume can be maintained despite increased counter pressure.
Illnesses & ailments
Heart disease can negatively affect the heart's activity and lead to a reduced stroke volume. If the heart is no longer able to carry the amount of blood required by the body, it is called heart failure. Heart failure can be divided into a chronic and an acute course. In addition, a distinction can be made between left heart failure, right heart failure and global insufficiency.
Acute heart failure develops within a few hours or days. Possible causes are pulmonary embolism, heart attack, pericardial tamponade or valve insufficiency. Chronic heart failure develops rather slowly. Possible causes of chronic heart failure are lung disease or high blood pressure. The symptoms depend on the location of the insufficiency.
In the case of insufficiency of the left heart, the insufficient heartbeat volume causes the blood to back up in the vessels of the lungs. Characteristic symptoms are cough and shortness of breath. In the worst case, pulmonary edema develops. The impaired performance of the heart also leads to reduced performance and low blood pressure.
In right heart failure, the blood backs up into the body's circulation. The increased venous pressure leads to an escape of water into the tissue. The result is edema in the legs, ascites or a pulmonary effusion (pleural effusion). In global heart failure, the right and left hearts are affected. Symptoms of left and right heart failure appear.
Stroke volume can also decrease if the heart is inflamed. When it comes to inflammation, a distinction can be made between pericarditis, myocarditis and endocarditis. Several layers of the heart are often affected at the same time.
When the heart muscle is inflamed, the myocardium is inflamed. Infectious myocarditis is usually caused by an infection with viruses. Heart muscle inflammation is often preceded by a rather mild viral infection, such as a cold. Bacteria can also lead to inflammation of the heart muscle. Non-infectious heart muscle inflammation is usually autoimmune. The inflammation restricts the heart's pumping capacity and thus also reduces the heartbeat volume. The main symptom of myocarditis is therefore restricted and reduced performance. Those affected tire more quickly and feel weak. Endocarditis and pericarditis show similar symptoms. Pericarditis can also be accompanied by pain.
All inflammations of the heart are dangerous and in the worst case scenario can be fatal. With consistent physical restraint and early therapy, the prognosis is good.












.jpg)

.jpg)
.jpg)











.jpg)