The Hippel-Lindau syndrome is a hereditary benign tumor disease primarily of the retina and the cerebellum. It is based on a malformation of the blood vessels. Other organs can also be affected.
What is Hippel-Lindau Syndrome?

© deagreez - stock.adobe.com
The Hippel-Lindau syndrome is a very rare benign, lumpy tissue change mainly in the area of the retina and the cerebellum. So-called angiomas (blood sponges) occur as tumors. This is why the disease is often called retinocerebellar angiomatosis designated. The brain stem and spinal cord are also often affected.
The tumors develop from preforms of the connective tissue and consist of blood vessels. They are mostly benign, but can also degenerate maliciously. Sometimes tumors are found in the pancreas, adrenal gland, epididymis, or kidneys. Kidney tumors in particular can develop into cancer more often. The disease was named after the German ophthalmologist Eugen von Hippel and the Swedish pathologist Arvid Lindau. In 1904 von Hippel discovered angiomas in the retina of the eye.
22 years later, in 1926, Arvid Lindau described angiomas in the spinal cord. In addition to the name Hippel-Lindau syndrome, the disease is also under Von-Hippel-Lindau-Czermak syndrome, Hippel-Lindau disease, retinocerebellar angiomatosis or Retinal angiomatosis known. It is a neurocutaneous syndrome, which is characterized by vascular malformations in various organs. Neurocutaneous syndromes are diseases that manifest themselves in the skin and central nervous system.
causes
The Hippel-Lindau syndrome is genetic. The disease is inherited as an autosomal dominant trait. However, the severity of the syndrome also depends on many other factors. Although the genetic defect is passed on to the next generation, the severity of the disease varies within the family. A spontaneous mutation occurs in 50 percent. So half of the sick in the family have no hereditary problems.
However, this means that several mutations in the HL gene on chromosome 3 can be responsible for the development of the disease. This gene has a major influence on the development of blood vessels and the cell cycle. It is not just a mutation in the HL gene that leads to dysregulation of the blood vessels. It has now been established that when the disease breaks out, there are a number of mutations that are distributed across the entire gene.
Symptoms, ailments & signs
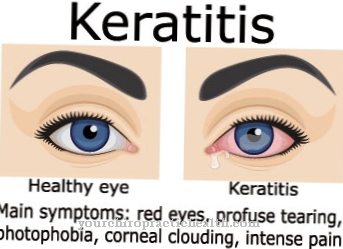
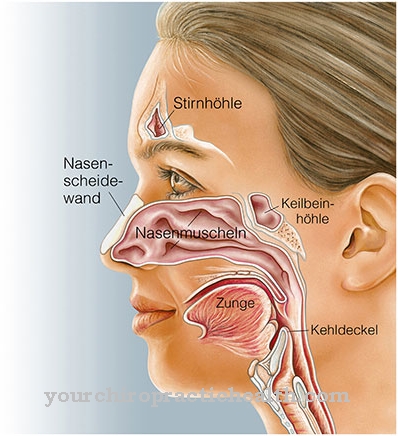
The Hippel-Lindau syndrome generally manifests itself in exhaustion, high blood pressure and headaches. In addition, there are neurological symptoms such as balance disorders, disorders of movement coordination or signs of intracranial pressure. Visual disturbances (visual disturbances) are often the initial symptoms. The symptoms are, however, largely dependent on the size and location of the tumors.
Angiomas are usually found in the retina, in parts of the central nervous system, in the spinal cord or in the brain stem. The cerebrum is rarely affected. Examinations often reveal malformations in other organs as well. Cysts are found especially in the pancreas, liver or kidneys. Benign arteriovenous vascular malformations are also present in the liver. When the adrenal glands have an angioma, a pheochromocytoma develops.
There are forms of Hippel-Lindau syndrome with and without pheochromocytoma. The pheochromocytoma is a benign tumor of the adrenal gland that produces an increased amount of the hormones adrenaline and noradrenaline. Heart rate and blood pressure are increased. The blood pressure rises at intervals and reacts particularly strongly in stressful situations.
Diagnosis & course of disease
The detection of multiple hemangiomas in the retina of the eyes is clear evidence of the Hippel-Lindau syndrome. A family history provides information about any accumulation within the family or relatives. Imaging procedures can detect possible tumors in the kidneys, adrenal glands, pancreas or liver.
Complications
Various organs can be affected by Hippel-Lindau syndrome. In most cases, however, the person concerned suffers from a general feeling of illness. This leads to a severe headache and the affected person looks exhausted. Furthermore, high blood pressure occurs, which in the worst case can lead to a heart attack. The patient also complains of impaired vision and restricted mobility.
The patient's coordination can also be disturbed by Hippel-Lindau syndrome. In many cases, the Hippel-Lindau syndrome also has a negative effect on the patient's behavior, so that it is not uncommon for them to become adept. The heart rate increases even in simple and easy situations, so that stressful situations can lead to sweating or panic attacks for the person concerned. Without treatment for Hippel-Lindau syndrome, life expectancy is usually reduced.
The syndrome cannot be treated in every case. This is especially true if the syndrome is genetic. Symptomatic treatment can, however, limit the symptoms and possibly remove the tumor. The exact course of the disease depends on the severity of the tumor. The life expectancy of the patient may therefore also be limited.
When should you go to the doctor?
In the event of a general feeling of illness, malaise or fatigue, close self-observation should be carried out. If fatigue persists despite a restful night's sleep, this is a sign of a health problem. If the symptoms persist for several weeks, there is a reason for a check-up. If symptoms spread or if they intensify, a doctor should be consulted. Consult a doctor in the event of increased blood pressure, impaired coordination or motor movement sequences.
If the blood pressure rises unusually, especially in stressful life situations, a doctor's visit is necessary. If there is a feeling of pressure inside the head, headaches, visual disturbances or a limitation of the auditory system, there is cause for concern. In severe cases, there is complete hearing loss. This should be examined and treated as soon as possible. Problems in the area of the back, a decline in physical performance and a diffuse pain experience should be clarified by a doctor.
If the symptoms appear for no reason, the person concerned needs a medical examination. In the event of functional disorders of the gastrointestinal area, experience of heat or fluctuations in mood, a consultation with a doctor is recommended. Discomfort in the kidney region or abnormalities when urinating are considered warnings from the body that should be followed up.
Doctors & therapists in your area
Treatment & Therapy
Since Hippel-Lindau syndrome is a genetic disease, a causal treatment is not possible. However, existing angiomas can be removed by a variety of procedures. These include laser caogulation, cryotherapy, brachytherapy, transpupillary thermotherapy, photodynamic therapy, radiation therapy, proton therapy or drug treatment. In laser therapy, smaller angiomas are denatured by local overheating. The diseased tissue dies and heals at this point.
Cryotherapy uses temperatures as low as minus 80 degrees to freeze peripheral angiomas in the retina. In brachytherapy, radioactive radiation is used to destroy angiomas. Transpupillary thermotherapy can be used for retinoblastomas, choroidal melanomas, or choroidal hemangiomas. It works on the basis of heating the tumor with infrared radiation. In the case of angiomas, the presentation of treatment success is contradictory. Some studies have reported success in treating angioma. In other studies, the treatment was ineffective.
In photodynamic therapy, light is used in combination with a light-active substance. Verteporfin is used as a light-active substance in current studies. An improvement in eyesight is noted. However, macular edema can occur. Radiation therapy does not show any significant results. Eyesight can be improved, but not all tumors shrink evenly. The best results are achieved with small angiomas. Proton therapy works with very high precision. It is used when the angiomas are near sensitive tissue.
Outlook & forecast
The prognosis for Hippel-Lindau syndrome depends largely on the type and location of the various tumors. The mean life expectancy was determined to be 50 years. However, life expectancy and quality of life can be significantly increased through early detection and treatment of the tumors. Although the tumors initially simply deform the connective tissue of the blood vessels and are benign, some of them can turn into malignant tumors. Kidney carcinomas, which are the main reason for the high mortality, then develop particularly frequently.
Pancreatic carcinomas (pancreatic cancer) and carcinomas of other organs also occur. Pancreatic cancer is one of the particularly aggressive tumors that can quickly lead to death. Another common cause of death is hemangioblastoma in the brain, which can lead to cerebral haemorrhage. General symptoms such as high blood pressure, headache and fatigue as well as neurological symptoms also depend on the individual tumors.
Some patients do not have symptoms if they have not already had hemangioblastomas in the central nervous system. Hemangioblastomas in the retina can lead to retinal problems as the disease progresses and can even lead to complete blindness. Furthermore, tumors that cause complete hearing loss are possible in around 10 percent of patients. The course of the disease can be so different that an exact prognosis for the individual affected is not possible.
prevention
There is no prevention of Hippel-Lindau syndrome because it is a genetic disease. If there is a familial accumulation of the disease, genetic counseling should be carried out if the child wishes to have children.
Aftercare
After being diagnosed with Hippel-Lindau syndrome, life changes for those affected. From now on you have to watch your body carefully and consult a doctor to clarify each new lump. The earlier masses are treated, the greater the likelihood of a successful treatment and the fewer the complications.
Patients must have regular checkups throughout their lives. Since new spatial demands can appear in the entire body, these must be carried out by doctors from different specialties. In annual general clinical examinations, all palpable masses are discussed, blood pressure is measured and further therapy is discussed. Annual ophthalmological examinations enable the early detection of retinal hemangioblastomas.
Collection urine is also checked annually, which can be used to diagnose pheochromocytomas. MRI examinations of the head and spinal cord are carried out every three years in order to image and treat spinal hemangioblastomas. An MRI of the abdomen also serves to rule out pheochromocytomas, renal cell carcinomas and pancreatic tumors.
The attending physicians may also use other examination methods such as positron emission tomography or single photon mission tomography or scintigraphy to supplement the diagnosis of the type and spread of tumors. In individual cases, a catheter examination of blood vessels may be necessary in order to obliterate the vessels leading to the tumor and to facilitate subsequent therapy.
You can do that yourself
With Hippel-Lindau syndrome, there are no special possibilities for self-help available to those affected. Unfortunately, the syndrome cannot be prevented or treated causally, so only symptomatic treatment is given. However, even after successful treatment, the patient is often dependent on regular examinations in order to diagnose and treat other tumors at an early stage.
The tumors are usually removed by surgery. The type of intervention depends strongly on the location and the severity of the tumor. As a rule, however, the life expectancy of the person affected is not reduced by Hippel-Lindau syndrome, since the tumors can be removed and are benign. Often psychological upsets or depression can be avoided by talking to other people affected or to close friends and relatives. Especially with children, an informative conversation should always take place in order to inform them about the possible consequences of the disease.
In most cases, treating Hippel-Lindau syndrome can also improve the affected person's eyesight. However, these are still dependent on visual aids in order to cope with everyday life. Due to the high blood pressure, stressful situations and strenuous sports or activities should be avoided. This protects the patient's circulation and heart.









.jpg)

.jpg)
.jpg)











.jpg)