Of the Hyperinsulinism is a condition of increased insulin concentration in the blood, which leads to hypoglycaemia (low blood sugar). Hypoglycaemia often causes serious health problems that can lead to coma or even death.
What is hyperinsulinism?

© designua - stock.adobe.com
It will be between Hyperinsulinism and hyperinsulinaemia. While the insulin concentrations are only temporarily increased in hyperinsulinemia, hyperinsulinism is characterized by permanently increased insulin values in the blood. There are several causes for the increased concentrations in the blood.
Most often it is a congenital hyperinsulinism, which is genetic and already exists from birth. Insulin as a hormone in the pancreas is responsible for regulating blood sugar levels. It ensures that glucose is transported into the body's cells. The more insulin there is, the more glucose is transported into the cells. The blood sugar level drops more and more and reaches too low values.
As a result, the body can no longer be supplied with sufficient glucose. The brain in particular is dependent on glucose. If the glucose supply to the brain becomes too low, it can no longer adequately perform important functions. In severe cases, coma and death often occur. In milder cases of hyperinsulinism, the body tries to compensate for the hypoglycaemia by eating more food.
causes
Hyperinsulinism can be caused either by a permanently increased production of insulin in the pancreas or by a delayed breakdown of insulin. Usually, however, more insulin is produced. For example, type II diabetes is caused by decreased insulin resistance.
This means that although there is enough insulin available, it is less effective due to the lack of insulin receptors. The pancreas now tries to balance the effectiveness of the insulin by increasing insulin production. In this case, however, the blood sugar level remains elevated or reaches maximum normal values.
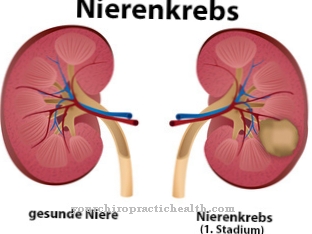
Hyperinsulinism with hypoglycaemia develops with a special tumor of the pancreas (insulinoma) or with a genetic overproduction of insulin. The so-called genetic congenital hyperinsulinism is the most common form of hyperinsulinism. This in turn can be divided into focal and diffuse hyperinsulinism.
In focal congenital hyperinsulinism, there is usually only one affected area in the pancreas. Diffuse hyperinsulinism is characterized by the fact that all islet cells produce more insulin. Insulin production can also be increased due to psychological influences or a slightly responsive pancreas.
Symptoms, ailments & signs
Hyperinsulinism is characterized by constant sweating, tremors and paleness. In congenital hyperinsulinism, these symptoms appear from birth. Behavioral problems, lethargy, seizures and impaired consciousness are also observed. The symptoms can be treated quickly with glucose.
After that, however, the blood sugar level drops again very sharply. In severe, untreated cases, the disease can be fatal or cause severe mental developmental disorders. In the very mild forms of hyperinsulinism, a constant feeling of hunger often leads to increased food intake. The result can be profound obesity.
Diagnosis & course of disease
The diagnosis of hyperinsulinism is made through blood tests. Insulin levels, fasting blood sugar in the blood and ketone bodies in the serum are measured. If the insulin level is above 3 U / l in the fasting state and the blood sugar level is low, this can be referred to as hyperinsulinism.
The concentration of the ketone bodies is reduced because insulin inhibits lipolysis and as a result fewer ketone bodies can arise from the breakdown of fatty acids. The improvement in symptoms by administration of glucose or the administration of glucagon also indicates hyperinsulinism. Finally, the pancreatic tissue can be assessed using imaging methods such as sonography.
In addition, sonography is also suitable for ruling out a tumor as the cause of hyperinsulinism. When assessing the pancreatic parenchyma, the aim is to distinguish focal from diffuse hyperinsulinism. The distinction is very important in designing the treatment strategy.
Complications
The hyperinsulinism leads to severe hypoglycaemia in the patient. This can lead to various health problems and complications. In many cases, hypoglycaemia makes people lose consciousness or feel sick and exhausted. The resilience of the person concerned drops considerably and the heartbeat increases even with light activities.
The affected person also looks pale and can hardly concentrate. Disturbances in consciousness occur and the patient suffers from sweating and seizures. The quality of life is severely restricted by hyperinsulinism. If the disease occurs in children, it can lead to significant developmental disorders, which can usually lead to secondary damage in adulthood.
The feeling of hunger is increased by hyperinsulinism and the patient tends to eat more, which can lead to obesity and overweight. There are no special complications in the treatment of the disease. Medicines are mainly used, which can eliminate the symptoms relatively quickly. Surgical intervention is only necessary in rare cases. Early treatment will not reduce the person's life expectancy.
When should you go to the doctor?
People who sweat quickly even with slight movements or performing everyday tasks should consult a doctor to clarify the symptoms. Nervousness, persistent trembling of the limbs, or a pale face are signs of an inconsistency. A doctor's visit is necessary as soon as the symptoms persist for several days or weeks and increase in intensity.
Cramp formation on the body, abnormal behavior or lethargy must be examined by a doctor. If the complaints already occur in a newborn child, the pediatrician must be informed immediately. In the event of a disturbance of consciousness or loss of consciousness, medical care must take place as soon as possible so that the survival of the person concerned is ensured. In severe cases, an emergency doctor should be called. Until the patient arrives, first aid measures must be taken and the breathing supply secured. A sudden breakdown, unexpected behavioral problems, or severe mood swings are cause for concern.
A visit to the doctor is advisable in the event of a decrease in the usual level of performance, reduced drive and inner restlessness. General weakness, feeling very hungry, and eating disorders should be discussed with a doctor. If there are irregularities in digestion, changes in weight or an increased need for sleep, the observations should be examined by a doctor.
Doctors & therapists in your area
Treatment & Therapy
Treatment of hyperinsulinism depends on its cause. Oral or intravenous substitution of glucose are considered conservative treatment methods. The hormone glucagon can also be substituted. Glucagon is the antagonist of insulin and ensures that the glucogen stored in the liver is broken down into glucose.
At the same time, drug treatment with diazoxide or nifedipine can be carried out. Diazoxide opens the ATP-sensitive potassium channels. Nifedipine inhibits the calcium channels. This inhibits insulin secretion. If the conservative methods do not improve the symptoms, surgical removal of the overactive islet cells can also be considered.
In focal hyperinsulinism, a complete cure is often possible. Here only the affected area of the pancreas is removed. In the case of diffuse hyperinsulinism, a complete resection of the islet cells would have to be carried out. In the process, however, type I diabetes develops. In this case, attempts are made to achieve the greatest possible success through drug treatment so that no operation is necessary.
However, it has been found that there is still an atypical hyperinsulinism that combines both forms of congenital hyperinsulinism. Atypical hyperinsulinism has several highly active sites in the pancreas. These can be detected using imaging techniques. Here, too, surgical removal of the affected areas may bring about complete healing.
Outlook & forecast
Hyperinsulinism causes serious complications if no medical care is obtained. The prognosis in these cases is extremely poor. Hypoglycaemia and severe life-threatening consequences occur. The patient may lose consciousness and fall into a coma. This condition is potentially life-threatening or can cause irreparable damage.
Treatment improves the chances of relief from the symptoms. However, the cause of the hyperinsulinism is decisive. In the case of a tumor, the stage and curability of the tumor are decisive for the overall prognosis. If the tumor is discovered early and completely removed, a good prognosis can be given with subsequent cancer therapy. In most cases, long-term therapy is initiated afterwards, during which the symptoms significantly improve. If there is no prospect of a cure with cancer therapy, drug treatment is used to alleviate existing symptoms. In these cases, the care of the patient is focused on the symptom relief of all irregularities in order to alleviate existing suffering.
If the patient suffers from an underlying chronic disease, no cure can be expected. The insulin balance is monitored and regulated. As soon as prescribed drugs are discontinued, the symptoms relapse. If the treatment plan is followed, there is a lasting improvement in the quality of life.
prevention
Most forms of hyperinsulinism cannot be prevented. Only the hyperinsulinism caused by type II diabetes mellitus can be prevented by a healthy lifestyle.
Aftercare
With hyperinsulinism, follow-up care is difficult in most cases. In most cases, the measures and options for follow-up care are severely limited, so that the person affected is primarily dependent on a quick and, above all, early diagnosis of this disease. In the worst case, if left untreated, the affected person can even die, so that early detection is the main focus of this disease.
The earlier the hyperinsulinism is recognized, the better the further course of this disease is usually. The disease is often treated by taking medication. It is important to ensure the correct dosage with regular intake in order to relieve the symptoms correctly and permanently.
If there are any questions or uncertainties, a doctor must always be consulted first. In the event of side effects or interactions, a doctor should be called first. Contact with other hyperinsulinism patients can be useful, as it is not uncommon for information to be exchanged. Whether the disease will lead to a reduced life expectancy cannot generally be predicted.
You can do that yourself
Hyperinsulinism must definitely be treated by a doctor. In the worst case, the patient can die without treatment.
In the case of diabetes, a healthy diet and lifestyle can have a very positive effect on the disease. Ideally, this can also completely limit the disease. As a rule, however, those affected are dependent on medical treatment. Since those affected sweat frequently and heavily due to the disease, light, airy clothing should be worn to avoid sweating.
In the case of behavioral problems or disorders of consciousness, special support for those affected can have a positive effect on the disease. However, the symptoms are treated relatively easily and quickly by taking medication. In addition, patients with hyperinsulinism should have regular blood tests to check blood sugar levels. Other examinations of the internal organs are also advisable.
In case of loss of consciousness due to hypoglycaemia, an emergency doctor should be called. Until the emergency doctor arrives, the person concerned must be brought into a stable lateral position. Regular and calm breathing should also be set.

.jpg)

.jpg)






.jpg)

.jpg)
.jpg)











.jpg)