A Hyperphosphatemia denotes too high a phosphate concentration in the blood. There are acute and chronic forms of this disorder. Acute hyperphosphatemia is a medical emergency and life-threatening, while chronic overloading with phosphate leads to cardiovascular diseases in the long term.
What is hyperphosphatemia?

© Ronald Rampsch– stock.adobe.com
The Hyperphosphatemia represents an increased phosphate concentration in the blood. The increase in the phosphate concentration can occur very quickly or over longer periods of time. Its rapid increase is called acute hyperphosphatemia. At the same time, there is a strong decrease in the calcium concentration (hypocalcemia), which leads to massive disruption of the electrolyte balance. This condition is extremely dangerous.
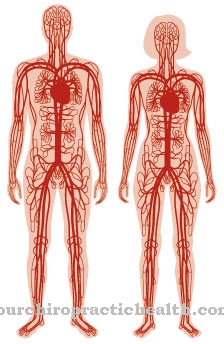
Chronic hyperphosphataemia is usually the result of impaired kidney function and does not initially cause any symptoms. In the long term, with this form of hyperphosphataemia, calcium deposits form in the blood vessels with the risk of heart attacks and strokes. Phosphate, calcium and bone metabolism are closely linked.
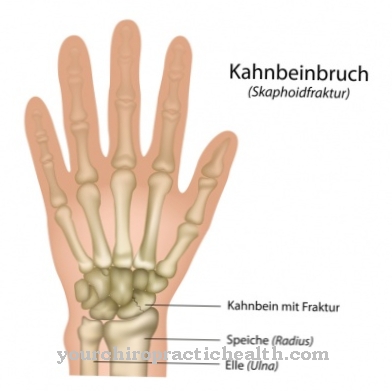
The bones consist of more than 80 percent calcium phosphate. In chronic hyperphosphataemia, in addition to calcification of the blood vessels, the bones also break down in the long term. The kidney is the most important organ regulating the phosphate concentration. It ensures that excess phosphates are excreted in the urine.
causes
Both in terms of cause and effect, acute and chronic hyperphosphatemia must be considered separately. In acute hyperphosphataemia, the phosphate intake is so massive that the kidney's capacity is by far exceeded. However, kidney function is normal. The phosphate supply can in turn be both exogenous and endogenous.
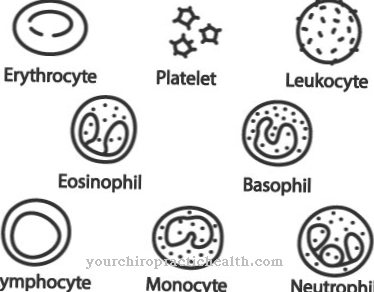
For example, solutions containing phosphate, which are used, for example, to cleanse the colon, can lead to acute hyperphosphataemia, especially in older people. Of course, this also applies to drinking phosphate solutions. However, the body's own causes also sometimes cause acute hyperphosphataemia. In the case of sudden necrosis of the body's own tissue or hemolysis, the phosphates of the dead cells are released.
If the kidney capacity is exceeded, acute hyperphosphatemia occurs. Chronic hyperphosphatemia almost always results from poor kidney function. The capacity of the kidneys to absorb phosphates is reduced. As a result, their concentration in the blood increases slowly. However, these processes are very complex. An increased phosphate concentration binds calcium with the formation of calcium phosphate.
The decreased calcium concentrations cause bone degradation to an increased extent via a feedback mechanism. The calcium phosphates are deposited as calcium-like salts in the blood vessels and lead in the long term to arteriosclerosis, heart attacks or strokes. However, there are also hormonal or genetic diseases which, despite normal kidney function, can lead to hyperphosphataemia due to increased reabsorption of phosphate from the primary urine.
These include hypoparathyroidism, acromegaly or familial tumorous calcinosis. Intravenous nutrition, bisphosphonate treatment, or vitamin D poisoning can also lead to hyperphosphataemia. In addition, more phosphates accumulate in chemotherapy, acute leukemia or diabetic ketoacidosis.
Symptoms, ailments & signs
Acute hyperphosphatemia is a very life threatening condition. The greatly increased phosphate concentrations simultaneously lead to a sharp drop in the calcium concentration in the blood. Calcium ions and phosphate ions immediately form poorly soluble salts from calcium phosphate. The resulting hypocalcemia disrupts the body's electrolyte balance.
Symptoms such as nausea, vomiting, diarrhea, seizures, muscle spasms, circulatory problems or irregular heartbeat occur. This can lead to sudden cardiac death. The chronic hyperphosphataemia does not cause any symptoms at first. In the long term, however, more and more calcium phosphate deposits form in the arteries, joints or organs.
The blood vessels can clog and stiffen. Heart attacks and strokes can occur over time. A rare but very painful and severe form of chronic hyperphosphataemia is so-called calciphylaxis. This leads to the death of skin tissue due to severe media calcification of the skin vessels. The fabric turns dark blue to black, mummifies and possibly falls off.
Diagnosis & course of disease
Laboratory tests for phosphates and calcium are carried out to clarify the hyperphosphatemia.
Complications
The hyperphosphataemia causes different symptoms in the patient. In most cases, this results in relatively high stress and discomfort in the heart, so that cardiovascular complaints can also develop. This limits the life expectancy of the patient and sudden cardiac death can lead to death of the person concerned.
In general, the patient feels sick and tired and suffers from severe exhaustion. Social contacts are also restricted and most patients withdraw from the hyperphosphataemia and no longer take an active part in life. Cramps can occur in the muscles, so that movement is also restricted. Most patients also suffer from vomiting and nausea.
It is not uncommon for severe diarrhea to occur, which also has a negative effect on the patient's everyday life. The diarrhea and vomiting result in a high loss of fluid. If this loss is not made up, it can lead to dehydration, which is very unhealthy for the body. Treatment usually takes place with the help of infusions and medication and can acutely relieve the symptoms. There are no further complications or special complaints.
When should you go to the doctor?
If symptoms such as nausea and vomiting, diarrhea, and seizures are noticed, the cause may be hyperphosphatemia. A doctor should be consulted if symptoms persist longer than usual. The disease is a life-threatening condition that requires emergency medical treatment in any case. That is why the rescue service should be alerted at the latest when there are clear warning signs such as circulatory problems or muscle cramps. If the victim loses consciousness, first aid must be provided. A longer hospital stay is then usually indicated.
People who suffer from vitamin D poisoning, acute leukemia, diabetic ketoacidosis or acromegaly are particularly at risk. There is also a risk of hyperphosphataemia in connection with intravenous feeding or biphisphonate treatment. Anyone who is one of these risk groups should go to a hospital immediately if they experience the symptoms mentioned. If in doubt, the attending physician can be contacted first. The disease requires clarification and treatment by a specialist in internal medicine. In severe cases, intensive medical care in a specialist clinic is indicated.
Doctors & therapists in your area
Treatment & Therapy
The treatment of hyperphosphatemia initially depends on whether it is acute or chronic. In the event of acute hyperphosphataemia, immediate action must be taken. Here the phosphate excretion is accelerated by an infusion of physiological saline solution. Dialysis treatment can also be performed.
In chronic hyperphosphataemia, in addition to treating the underlying disease, various measures must be taken to inhibit phosphate uptake and release or to promote phosphate binding. Chronic hyperphosphataemia only occurs at a late stage in kidney disease, so that a causal treatment is no longer possible here.
Therefore measures are taken to keep the phosphate concentration as low as possible by other treatment methods. A low-phosphate diet and various phosphate binders reduce the absorption of phosphate from food. By taking vitamin D, increased bone breakdown and thus the release of phosphate can be inhibited. It has been shown that treatment with phosphate binders and vitamin D can significantly increase the life expectancy of dialysis patients.
Outlook & forecast
The prospect of improving health in hyperphosphatemia depends on the underlying disease and the intensity of the symptoms. In an acute situation, there is a risk of death for the person affected without immediate intensive medical treatment. Dialysis treatment is necessary so that the symptoms can be alleviated. If the treatment is accepted by the organism, the condition of the person concerned improves at least temporarily. In the next steps, it is necessary to clarify the cause and draw up a treatment plan.
With a chronic underlying disease, the prognosis is usually poor. Since the hyperphosphatemia remains symptom-free for a long time, this makes diagnosis and treatment more difficult. Nevertheless, calcium deposits in the organism continuously increase and ultimately lead to an acute health condition. In addition to endangering life, life-long impairments and disorders can occur. The disease causes a breakdown of the bone substance and thus leads to a decrease in physical performance. The damage is irreparable, only the progression of the disease can be influenced. The overall quality of life is reduced and a restructuring of everyday life is necessary. The general condition of the patient can lead to sequelae and other diseases.
With an early diagnosis, causal treatment can be initiated in some patients. The phosphate balance is regulated and monitored. Here is the prospect of permanent relief or healing.
prevention
Hyperphosphatemia is always a consequence of an underlying disease or disorder. The chronic high phosphate concentration is mostly due to renal insufficiency. Kidney disease can have many causes. Often, however, they are also the result of a wrong lifestyle. Renal insufficiency often occurs together with diabetes mellitus, cardiovascular disorders, lipid metabolism disorders and obesity. It is therefore important to prevent these diseases through a healthy lifestyle, plenty of exercise and avoiding alcohol and smoking.
Aftercare
In many cases of hyperphosphatemia, the person affected has very few or no direct follow-up options available. The affected person is primarily dependent on a quick diagnosis, since the hyperphosphataemia can in the worst case lead to death of the patient. The earlier the disease is recognized, the better the further course of the disease is usually.
A doctor should be consulted at the first symptoms and signs of the disease. In most cases, drinking a saline solution can relieve the symptoms relatively well. However, dialysis is often necessary here. Those affected depend on the help and support of their own family, which can make life much easier.
It may also be necessary to take medication. Those affected should ensure that they are taken regularly with the correct dosage to alleviate the symptoms. The intake of phosphate from food should also be regulated. Despite treatment, hyperphosphataemia usually results in a significantly reduced life expectancy for the patient.
You can do that yourself
If the hyperphosphataemia is acute and severe, the person affected usually has no options for self-help. In this case, immediate medical help is necessary to avoid the death of the person concerned. The treatment is carried out by an emergency doctor or in a hospital by giving a saline solution as an infusion. The supply of phosphate must be interrupted in any case. Dialysis can also be done in emergencies to provide support.
If hyperphosphatemia is a chronic disease, the person affected should be careful not to take in too much phosphate through their diet. A diet plan or a conversation with a nutritionist can be very helpful here. The intake of vitamin D also has a very positive effect on the course of hyperphosphataemia and can alleviate the breakdown of bones.
Furthermore, phosphate binders must also be taken regularly, although a consultation with a doctor should take place first and foremost. In general, contact with other sufferers can also have a positive effect on the disease. This leads to an exchange of information, which above all can contribute to a correct diet.



.jpg)






.jpg)

.jpg)
.jpg)











.jpg)