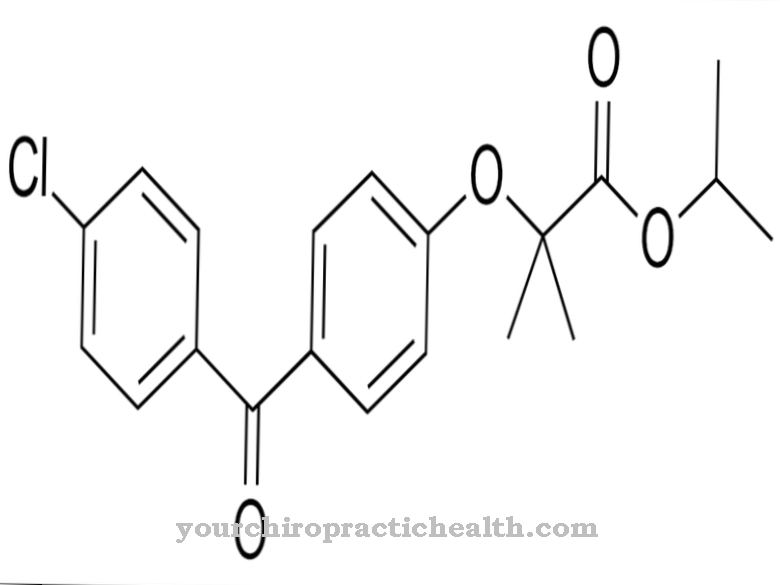
Indinavir belongs to the protease inhibitors. The medicinal substance is used to treat HIV infections.
What is indinavir?

Indinavir is an antiviral drug that belongs to the group of HIV protease inhibitors and is used to treat HIV infections. The HIV protease inhibitors are used as part of a special "Highly Active Antiretroviral Therapy" (HAART) together with other antiretroviral drugs such as NRTI (nucleoside reverse transcriptase inhibitors) and NNRTI (non-nucleoside reverse transcriptase inhibitors).
Indinavir was developed by the American pharmaceutical company Merck & Co and MSD Sharp & Drohme (MSD). The group developed oral dosage forms of the protease inhibitor, which were finally approved in 1996 by both the US FDA and the European Medicines Agency (EMA).
In the 1990s, indinavir was one of the most effective antiviral drugs. Over time, however, the drug has been increasingly replaced by more effective HIV protease inhibitors.
Pharmacological effect
Indinavir binds to the HIV viral protease. This is important for the pathogen to reproduce. The process leads to the inhibition of the viral enzyme, which in turn prevents the virus from multiplying. Finally, there is a decrease in the virus load.
The use of indinavir is more sensible in type 1 AIDS patients, as the drug has a greater affinity for HIV-1 than for HIV-2. In the bloodstream, approximately 60 percent of indinavir is bound to plasma proteins. The active substance is metabolized and broken down in the liver.
Indinavir has the disadvantage that the drug has to be taken every eight hours. This is the only way to ensure sufficient bioavailability. It is recommended that indinavir be taken either one hour before a meal or one hour after a meal. If the food is rich in proteins and fat, this results in a significant reduction in absorption. Doctors generally consider administration on an empty stomach to be sensible.
Medical application & use
Indinavir is used to treat adults, adolescents and children from the age of four for the treatment of HIV infections. The protease inhibitor is also suitable for post-exposure prevention in adults. Indinavir is not used as a single drug, which is due to the development of resistance in the HI virus. Instead, the drug is combined with other antiviral drugs. This can be zidovudine or lamivudine, for example.
The recommended dose of indinavir is 3 x 800 milligrams per day. With a lower dose there is a risk of considerable loss of effectiveness. However, the protease inhibitor must not be taken in larger quantities. The capsules are taken every eight hours with a glass of water or skimmed milk. Alternatively, it can also be served with tea, coffee or juice.
To counteract kidney stones, it is advisable to give the body at least six glasses of water a day. If the drug is to be administered with a meal, light meals such as corn flakes or toast with jam are recommended. It is also important to protect indinavir from heat and moisture.
Risks & side effects
The use of indinavir can sometimes have undesirable side effects. In around six percent of all patients, therapy has to be discontinued due to severe side effects. In most cases, digestive disorders such as diarrhea, abdominal pain, and nausea occur. The development of a bull's neck, in which there is an abnormal redistribution of fat in the neck area, is regarded as a rather rare undesirable side effect.
Other possible side effects are changes in the metabolism such as hyperglycaemia, hypercholesterolemia or hypertriglyceridaemia, headache, tiredness, feelings of weakness, bleeding in the case of hemophilia, skin rash, increased lipids, changes in taste perception, nephrotoxicity, sicca syndrome, which is associated with dry eye mucous membranes, dry mouth and skin, ingrown toenails, nail bed inflammation, hair loss and liver dysfunction. Kidney stones develop in up to 25 percent of all patients.
Indinavir must not be administered at the same time as certain other drugs such as benzodiazepines, cisapride, rifampicin, terfenadine, or astemizole due to interactions with the cytochrome system. This could lead to changes in blood plasma levels and severe side effects.











.jpg)

.jpg)
.jpg)











.jpg)