Under one ischemic colitis the doctor describes the condition of a change in the large intestine caused by inflammation. Sometimes, however, drugs can also trigger the inflammatory change.
What is ischemic colitis?
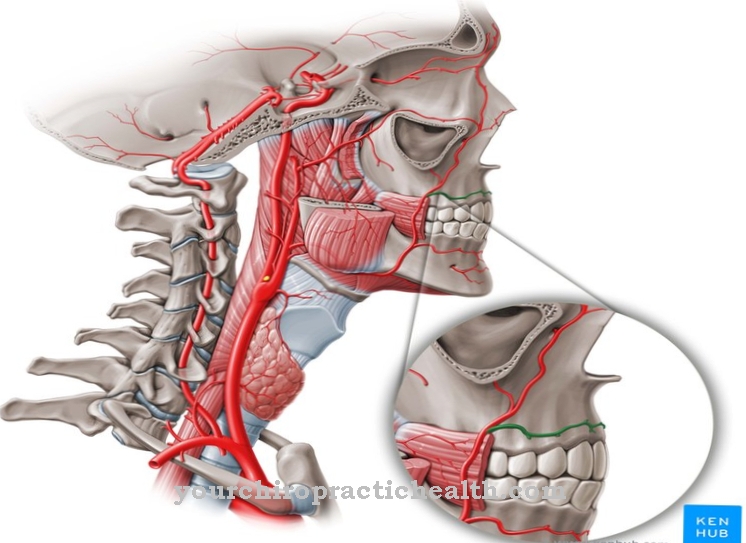
An inflammation of the large intestine, which results from a reduced blood flow to the intestinal mucosa, is what the doctor calls ischemic colitis. In many cases there is arteriosclerosis of the so-called mesenteric arteries and their branches. Ischemic colitis is particularly common in diabetics.
causes
The stenosing arteriosclerosis of the blood vessels that subsequently supply the large intestine with blood is the most common cause of ischemic colitis. But drugs can also cause ischemic colitis. The clinical picture appeared under the medication of appetite suppressants (Phenterminen), cardiac glycosides (Digitalis) as well as contraceptives, NSAIDs and chemotherapeutics (Vinca alkaloids and taxanes).
Even TNF-alpha inhibitors, which fall into the category of the newer drugs, can promote ischemic colitis. Metamphetamine and cocaine abuse have also been linked to ischemic colitis. But mechanical constrictions, caused by a volvulus, braids or tumor, inflammatory swellings or an aortic aneurysm, which can occur after an operation, promote the formation of ischemic colitis.
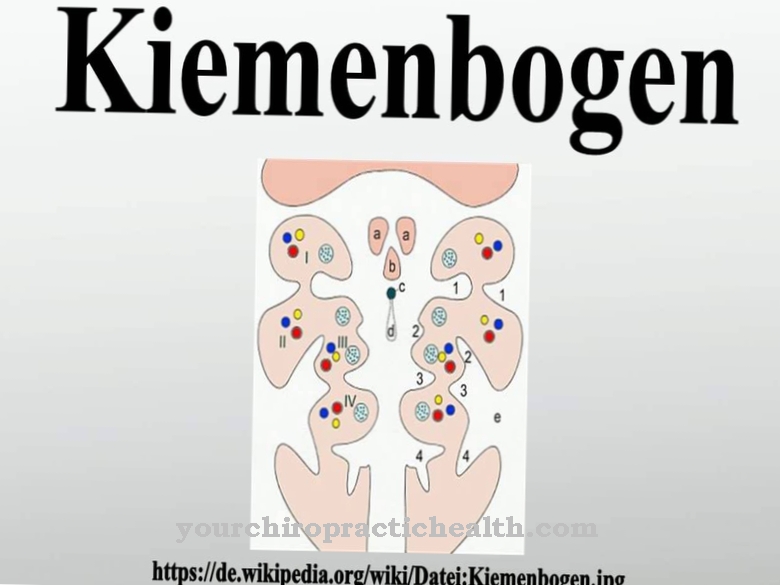
Another reason can be vasculitis. If there is a congenital system anomaly, which is located on the Drummond Arcades and the Riolan anastomosis, there is a significantly increased risk of developing ischemic colitis. Protein C deficiency, AT3 deficiency or factor V disease and the prothrombin mutation can also be causes of ischemic colitis.
The disease was also documented in connection with top athletes; Excessive marathons in particular can lead to ischemic colitis.
Symptoms, ailments & signs

As part of the diagnosis, the doctor performs a colonoscopy.
© Kateryna_Kon– stock.adobe.com
The complaints and symptoms are unspecific and can be compared with those of other colitis. Very mild forms manifest themselves mainly in that the patient suffers from very thin stools or diarrhea. Colon cramps are also possible. However, if there is a severe and pronounced form of ischemic colitis, there may also be amounts of blood in the stool.
However, the haematocracy is relatively untypical. The patient's abdomen is soft on palpation, although sometimes - in severe cases - defensive tension is possible, which suggests a peritonitis that has migrated through. If there is a necrotizing course, fever and chills develop. That form of ischemic colitis has a high mortality; here the doctor usually has to operate immediately.
Diagnosis & course of disease
As part of the diagnosis, the doctor performs a colonoscopy. Depending on the severity, the picture of the colonoscopy varies; Sometimes it can even be suspected that ulcerative colitis is present. In a few cases, the doctor also recognizes individual longitudinal ulcerations. Although these are characteristic, they can sometimes hardly be differentiated from Crohn's disease.
It is important that differentiation is made through histology. Thus, Crohn's disease and ulcerative colitis must be ruled out before the medical professional can diagnose ischemic colitis. If there are severe cases of ischemic colitis, imaging tests such as bowel sonography or computed tomography can also help explain the exact condition of the disease. The intestinal wall is already thickened; Sometimes the doctor can also detect gas formation in the intestinal wall (so-called pneumatosis coli).
Ischemic colitis disappears after two to three days. However, the course of the disease can also bring complications. For example, tissue can die or persistent bleeding caused by a perforation of the intestine can occur. Other complications include bowel inflammation and intestinal obstruction.
Complications
In most cases, this disease causes symptoms or complications in the stomach and intestines. Those affected often suffer from diarrhea and nausea. The quality of life is also significantly reduced by this disease. Furthermore, there are severe cramps in the stomach and abdomen, and in some cases bloody stool occurs.
Not infrequently, loss of appetite is also noticeable, which can lead to underweight or deficiency symptoms. Those affected can also suffer from chills or fever. If there is no immediate treatment, the person affected can also die of this disease. Furthermore, it can lead to an intestinal obstruction or inflammation in the intestine.
The treatment of this disease takes place with the help of antibiotics and can alleviate the symptoms. There are no further complications. In severe cases, however, surgery may be necessary. This can also lead to heart problems or diabetes. As a rule, it cannot be predicted whether this will reduce life expectancy.
When should you go to the doctor?
Ischemic colitis heals on its own in many cases. A doctor should be consulted if typical symptoms such as intestinal cramps, pain in the epigastric region or diarrhea persist for more than a week. If further symptoms arise, medical advice is required in any case. If you have a fever or chills, it is best to consult your doctor. Blood in the stool is also a clear warning that needs to be clarified quickly.
People with vasculitis or cancer are particularly prone to developing ischemic colitis. Likewise, patients who regularly take appetite suppressants or who suffer from a protein deficiency. Anyone who belongs to these risk groups must immediately discuss the symptoms with the responsible doctor. Medical help is required at the latest when the patient becomes underweight as a result of the symptoms. The person concerned should see a general practitioner or gastroenterologist. Children are best brought to a pediatrician or the nearest clinic on the same day.
Therapy & Treatment
In many cases the patient does not need any different therapy; ischemic colitis heals spontaneously. If treatment is given, the doctor decides which form of the disease is present. In the case of mild forms of the disease, which should usually disappear after two to three days, the doctor can prescribe antibiotics to prevent infection.
Occasionally, if you are dehydrated, intravenous fluids can be helpful. Medication that has the effect of constricting blood vessels should be discontinued (such as migraine medication or hormonal tablets). In the case of mild forms, the physician focuses primarily on alleviating the symptoms.
The doctor will then plan what are known as follow-up colonoscopies so that, on the one hand, he can monitor the healing process and, on the other, can react in good time if any complications arise. However, if there is a severe form of ischemic colitis that has already resulted in damage to the intestine, surgery can sometimes be performed.
As part of the operation, the doctor removes dead tissue, can repair a perforation in the intestine or sometimes create a bypass so that the bowel artery is no longer blocked. In a few cases, the doctor also removes part of the colon.
However, operations are rarely necessary. Favorable factors that negatively influence the course of the disease and make an operation necessary are diabetes mellitus, heart disease of any kind or low blood pressure.
Outlook & forecast
The prognosis for ischemic colitis is favorable in most patients. Spontaneous healing is often observed in this disease. Under normal circumstances, a clear relief of symptoms or freedom from symptoms are documented within 2-3 days. In a majority of the cases, there are no long-term complications or irregularities. In the short term, various complaints can be documented that cause a deterioration in quality of life. Ischemic colitis can recur in the course of life.
If the illness is caused by the administration of medication, the situation improves immediately after the medication is discontinued. In cooperation with the attending physician, alternative treatment methods must be discussed so that the existing underlying disease can be treated further.
One of the problems with ischemic colitis is how to differentiate it from other diseases. The diagnosis is difficult due to parallel complaints to other diseases of the intestine. In patients who have already been diagnosed with other pre-existing conditions, the general state of health must be taken into account for the prognosis. With chronic illnesses such as diabetes or with an existing heart disease, the prognosis worsens overall. In rare cases, surgery may be required. This is associated with the usual risks and side effects. If there are no complications, an improvement in health can be expected.
prevention
Due to the fact that the development of ischemic colitis cannot always be clarified, no specific preventive measures are known to prevent the disease. It is advisable - if the patient is one of the risk groups - to avoid drugs that serve the purpose of reducing the blood flow.
Furthermore, regular exercise and an examination of the colon is recommended if underlying diseases such as diabetes mellitus or any diseases of the heart are known.
Aftercare
The risk of ischemic colitis can be reduced by avoiding certain medications during follow-up care. Anyone who belongs to the risk group should therefore have their medication setting checked by their doctor and changed if necessary. In this way it is possible to restrict the current blood flow. In the period after the treatment, those affected can support the recovery process by changing their own habits.
Regular activities and close monitoring of existing underlying diseases are recommended for this. These are typically diabetes or heart problems. Sometimes there is spontaneous healing so that further therapy is not necessary. In other cases that don't go so well, the doctor will often prescribe antibiotics.
The patient takes this exactly as prescribed. A certain amount of care, warmth and a healthy diet rich in vitamins help to strengthen the body. The patient should also drink enough fluids to avoid dehydration. Regular doctor's appointments ensure constant monitoring.
Alternative natural remedies often help with complications such as intestinal cramps or diarrhea. Before taking it, it makes sense to discuss it with your doctor. Mild remedies such as herbal tea can also be used without medical advice to treat mild gastrointestinal complaints.
You can do that yourself
In some cases, ischemic colitis heals spontaneously and does not require further treatment. If the outcome is less positive, antibiotic treatment is indicated. This can be supported by some measures by the person concerned.
In general, the patient should take it easy and pay attention to a healthy and balanced diet. It is especially important to drink a lot to prevent dehydration. In addition, regular visits to the doctor are necessary. The triggering drug may have to be discontinued or adjusted differently. If symptoms such as diarrhea or intestinal cramps occur, alternative remedies from natural medicine are recommended. In consultation with the doctor, preparations with arnica or devil's claw, for example, can be used. Soothing herbal teas and other gentle remedies may also be used without the consent of the doctor and help especially with less pronounced gastrointestinal complaints.
If you have a fever and chills, bed warmth and rest are recommended. The patient should take their body temperature regularly and consult a doctor if it rises suddenly. In general, if symptoms are severe, medical clarification is required to avoid further complications and to ensure a quick recovery.

.jpg)

.jpg)
.jpg)

.jpg)