Cardiomyopathy is the technical term for acute and chronic diseases of the heart muscle. For the layman, the causes of cardiomyopathy are almost unmanageable.
What is cardiomyopathy?

© matis75 - stock.adobe.com
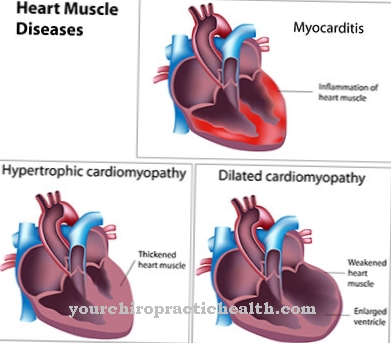
Under Cardiomyopathy the medical professional understands a wide range of Heart muscle disease. The term excludes the causal involvement of a heart valve defect or the pericardium.
The diverse manifestations of cardiomyopathy led to various classifications in specialist science. However, a division into 2 groups is increasingly gaining ground:
1. Primary cardiomyopathy: The underlying disease affects the heart muscle itself.
2. Secondary cardiomyopathy: The underlying disease does not come from the heart muscle, but is a regular or possible complication due to a disease in one or more other organs.
This definition does not take into account whether the cause is genetic or due to external factors. Both hereditary and acquired heart muscle diseases belong to the spectrum of primary and secondary cardiomyopathy.
causes
The primary cardiomyopathy is often the result of an inflammation of the heart muscle (myocarditis). This includes the well-known flu myocarditis and autoimmune diseases in the course of pregnancy. Several causes, certainly also genetic factors, come together in the case of heart failure (cardiac muscle weakness). Other cardiomyopathies are based exclusively on genetic defects in the heart muscle fibers or the neuronal cardiac conduction system.
Secondary cardiomyopathies include clinical pictures that can be traced back to a vitamin deficiency or a deficit of trace elements. Chemotherapy, stimulants or heavy metals can also damage the heart muscle. Furthermore, it is diseases of the nervous system and diseases from the rheumatic type that can lead to secondary cardiomyopathies.
Metabolic diseases often result in degradation products being deposited in different parts of the body. This also results in some of the secondary cardiomyopathies. Among the hormone disorders, the overactive and underactive thyroid are the triggers; diabetes is also known as the cause of cardiomyopathy.
Symptoms, ailments & signs
Cardiomyopathy often goes without symptoms for many years. As the heart muscle disease progresses, there are increasing complaints that significantly impair the performance and well-being of the person concerned. Typical symptoms of cardiomyopathy include tiredness and physical exhaustion as well as shortness of breath during exercise.
The shortness of breath is hardly noticed at the beginning and often subsides after a few minutes. Later, however, the breathing difficulties also occur at rest and thus lead to severe malaise, panic attacks or even fear of death. This is accompanied by chest pain, which is mainly noticed after eating, after consuming alcohol and when exercising, and which later also occur permanently.
The lack of oxygen in the organs also causes fluid to build up in the legs and lungs. In the further course it can lead to cardiac arrhythmias and fainting attacks. Other possible consequences of cardiomyopathy are lung infarcts, strokes, and sudden cardiac death.
Those affected can recognize a heart disease by the typical, mostly hard and irregular heartbeats. In addition, blood pressure fluctuations can occur, which lead to dizziness and [[circulatory disorders9]. If the disease is recognized early and treated comprehensively, the progression of the symptoms can be prevented.
Diagnosis & course
To Cardiomyopathy the doctor will investigate if symptoms such as shortness of breath, easy fatigue or dizziness are present. First of all, an EKG shows the first abnormalities, which can also include cardiac arrhythmias.
Some forms of cardiomyopathy show an enlargement of the heart on x-rays. An ultrasound examination provides insights into the beating heart (echocardiography). Finally, exploration with the cardiac catheter provides clues about the serious disease.
Acute myocarditis, for example, has a good chance of recovery. As a rule, cardiomyopathies are progressive degenerative diseases that are associated with a decrease in the pumping capacity. In the last stage, cardiac arrest (sudden cardiac death) is often the result of cardiomyopathy.
Complications
Cardiomyopathy causes complaints and diseases of the heart muscle. The life expectancy of the person affected is usually limited and the patient can die of the complaints if these complaints are not treated in good time. Most of the time, the patient's resilience drops significantly and those affected suffer from shortness of breath.
Certain activities or sporting activities are no longer possible due to cardiomyopathy. It comes to disturbances of the heart rhythm and in the further course to a heart failure. If left untreated, this can lead to patient death. Likewise, heart problems often lead to water retention in the legs or stomach. Patients often experience dizziness or loss of consciousness. If left untreated, the patient can also experience sudden cardiac death.
The treatment of cardiomyopathy is causal and depends on the underlying disease. The further course of the disease depends heavily on its severity, so that it is not possible to predict a general course of the disease. In some cases, a heart transplant is also necessary so that the person can continue to survive.
When should you go to the doctor?
People who experience recurring breathlessness or water retention in their legs may have cardiomyopathy. A doctor's visit is indicated if the symptoms persist after a few days or if other symptoms appear. Cardiac arrhythmias and fatigue should be clarified quickly in order to avoid serious complications. People who also suffer from dizziness and impaired consciousness should call an ambulance or be admitted to hospital. The same applies to severe pain, skin changes and cramps.
Cardiomyopathy is often associated with inflammation of the heart muscle or heart failure. A vitamin deficiency, chemotherapy or the consumption of luxury foods can also damage the heart muscle. Anyone who belongs to these risk groups should consult the responsible doctor. The GP can make an initial diagnosis and then refer the patient to a cardiologist. Depending on the cause of the disease, a specialist in internal medicine, a sports doctor or a psychologist can also be called in.
Treatment & Therapy
The secondary cardiomyopathies are initially treatable within the framework of the underlying systemic disease. The aim is, for example, to compensate for metabolic disorders or to detoxify in the event of intoxication. Myocarditis is fought with antibiotics and anti-inflammatory drugs.
In every chronic case, the cardiologist will focus his efforts on the symptoms of the weakening heart and will initiate appropriate medication. Cardiac glycosides (digitalis) have long been tried and tested for strengthening the heart, and lowering blood pressure is sought. The well-known beta blockers relieve the heart. The direct consequences of cardiomyopathy are also the focus of treatment.
Against edema (water retention in the tissue), diuretic drugs must be prescribed. Antiarrhythmic drugs are supposed to eliminate the atrial fibrillation that often occurs, sometimes only the implantation of a pacemaker helps. Anticoagulants reduce the risk of thrombosis and embolism. These are drugs to reduce the tendency to clot blood, with which in the course of cardiac arrhythmias are specifically to prevent strokes.
If the course of cardiomyopathy with advanced heart failure threatens to become life-threatening, a heart transplant is often the only solution. An artificial heart or electro-mechanical cardiac support systems can keep the patient alive until a suitable donor heart is available. Despite the best efforts of modern medicine, many patients ultimately die from the effects of cardiomyopathy.
Outlook & forecast
In order to achieve an improvement or even a significant slowdown in the course of the disease, the medically prescribed treatment and therapy plan must be strictly adhered to.
In so far as the cause of the disease is not genetic, the patient himself can achieve an improvement in quality of life with specific measures and support medical therapy. In cases in which an unhealthy lifestyle with an unbalanced and often excessive diet is the trigger of the disease, this must be urgently corrected. A change in diet has a positive effect on the circulation, relieves the heart and strengthens the immune system. Any weight reduction that may be necessary is also easier to achieve as a result. The changeover should be accompanied by both the attending physician and a nutritionist, so that it is tailored as best as possible to individual needs.
To relieve the cardiovascular system, it is advisable to completely avoid addictive substances such as alcohol and nicotine. The consumption of coffee should also be restricted and limited to a few cups per day. Regular exercise in everyday life, on the other hand, strengthens the circulation and improves the condition. Training with an ergometer or similar sports equipment is also beneficial.
The avoidance of excessive stress is a decisive point for both acquired and illness-related causes, as this favors the development of cardiomyopathy.
prevention
The Cardiomyopathy offers prophylaxis options despite the various causes. A moderate consumption of stimulants such as alcohol or nicotine is advisable here. It is also well known that exercise prevents several heart diseases at the same time. Foci of inflammation should be under medical supervision as soon as possible, this is especially true for flu and flu-like infections. Because this sometimes results in cardiomyopathy through the infection of the heart.
Aftercare
In most cases, the options for follow-up care for cardiomyopathy are very limited, so that those affected with this disease should ideally consult a doctor very early so that early treatment can be initiated. Self-healing cannot occur with cardiomyopathy, so that a doctor should be contacted at the first signs or symptoms of the disease.
With this disease, those affected are usually dependent on taking various medications. The correct dosage and regular intake of the medication must be observed in order to properly alleviate the symptoms. If antibiotics are taken, they must not be taken together with alcohol, otherwise their effect will be significantly reduced.
Likewise, the person affected with cardiomyopathy should undergo regular checks and examinations by a doctor in order to detect further damage to the heart at an early stage. Exhausting or stressful activities should be avoided with this disease. The further course of the cardiomyopathy is very much dependent on the time of diagnosis. In some cases, the life expectancy of those affected is reduced by this disease.
You can do that yourself
Patients who have been diagnosed with cardiomyopathy should take the condition seriously and follow their doctor's therapy plans and recommendations. In many cases, there are treatment methods that can improve the clinical picture. In other cases, slowing down or stopping the course of the disease is entirely possible.
For patients, this means that they have to consciously align their everyday life with the demands of the disease. Cardiomyopathy is often the result of an unhealthy lifestyle. If a wrong, unbalanced and mostly excessive diet has taken place over the years, a change in diet guided by a doctor can have a positive effect on the heart and circulation. In many cases, sensible weight reduction also contributes to better well-being in everyday life. Consumption toxins such as nicotine and alcohol should be avoided as far as possible, the consumption of coffee can be restricted. Incorporating regular exercise into everyday life and thereby carefully strengthening the cardiovascular system and stamina usually has a beneficial effect on health.
But these factors are not always the trigger for cardiomyopathy. Often this is also simply genetic and occurs even though the patient followed a healthy and active lifestyle. Excessive stress, for example at work or in the family, promotes the development of the disease. Patients should be aware of these risks and avoid them as best they can.

.jpg)

.jpg)

.jpg)






.jpg)

.jpg)
.jpg)











.jpg)