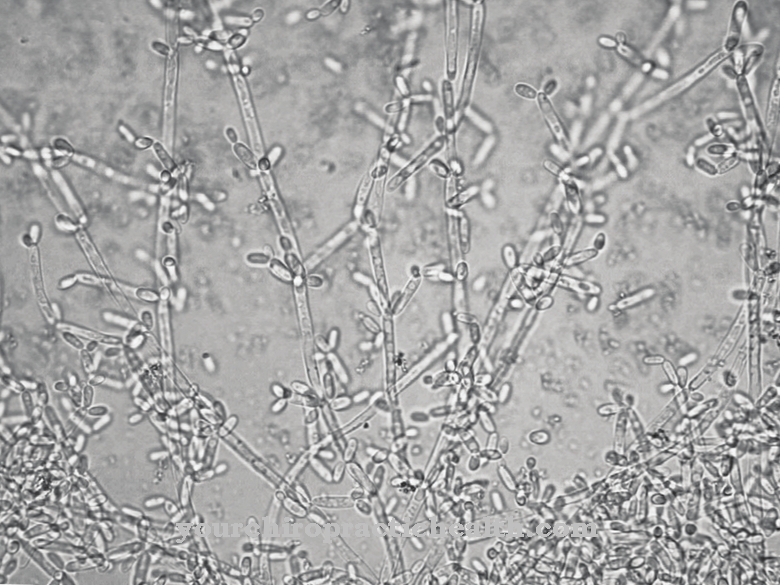
Legionella are rod-shaped bacteria of the Legionellaceae family flagellated on one of the poles. The bacteria are almost omnipresent and are mainly found in freshwater reservoirs, but have also been detected in salt water. They are the cause of the legionnaires' disease associated with severe pneumonia (also legionellosis) and the so-called Pontiac fever, a milder form of legionellosis without pneumonia.
What are legionella?
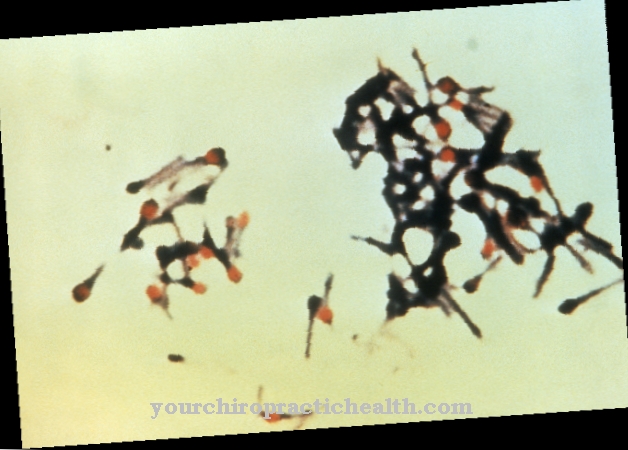
Legionella of the Legionellaceae family are rod-shaped, gram-negative bacteria with different lengths from about 2 to 5 micrometers. Of the more than 48 known species, the bacterium Legionella pneumophila is the main cause of Legionnaires' disease and Pontiac fever. In about 90 percent of the cases of Legionnaires' disease or Legionellosis, this bacterium is the causative pathogen.
The aerobic, non-spore-forming bacteria are mostly monopolar with one or more flagella. This means that they can actively move around. Legionella are also able to form biofilms that offer protection against unfavorable environmental conditions and against biocides.
The bacteria are dependent on amino acids for energy production because they cannot metabolize sugar, for example. The presence of cysteine and ferric ions is required for the preparation of amino acids. The bacteria are sensitive to dehydration and can only survive for a few minutes at temperatures above 60 degrees Celsius.
Occurrence, Distribution & Properties
Species of bacteria from the Legionellaceae family occur worldwide. The aerobically living bacteria mostly colonize surface waters and water reservoirs. Some species are also found in the soil. In mostly low concentrations, they can even be detected in groundwater. Legionella are partially resistant to salt water, as has now been proven.
Some species, such as Legionella pneumophila, are pathogenic. They are the main causes of Legionnaires 'Disease or Legionellosis, which was first described in 1976 during a Legionnaires' meeting in Philadelphia, USA. At that time, the transmission route was mainly the contaminated air conditioning of the hotel where the meeting took place.
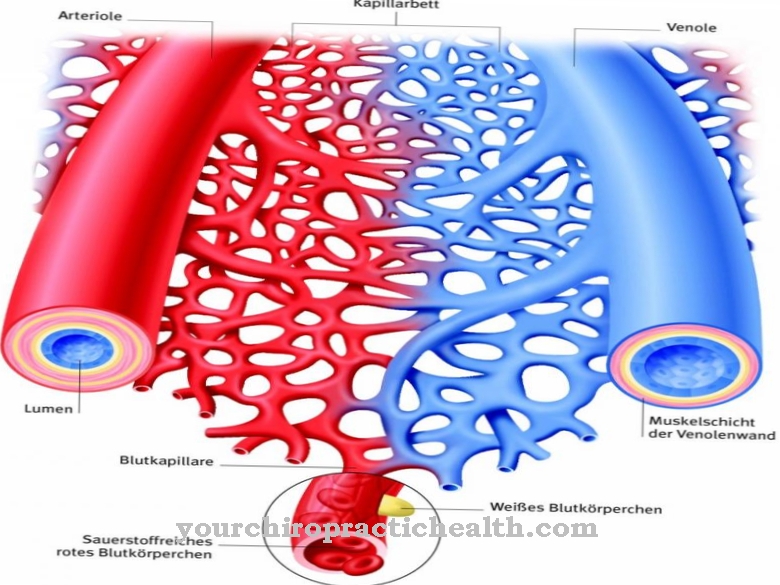
In the case of acute pneumonia as a result of an infection with Legionella, spread and infection usually takes place via droplet infection, as is the case with many other lung diseases. There is an increased risk of infection in the hot water area of swimming pools, i.e. under showers and in whirlpools, because the bacteria find optimal conditions at temperatures in the range of 30 to 50 degrees Celsius.
Since legionella rely on amino acids as well as the presence of the sulfur-containing amino acid cysteine and iron III ions for their energy supply, the bacteria are often associated with autotrophic iron manganese bacteria.
Amoebas also play a role in the spread of Legionella pneumophila. Although the bacteria are phagocytosed by the amoeba, they escape lysis. They can multiply inside the amoeba and are relatively well protected against poisons and disinfectants. Amoebas, which are known to cause amoebic dysentery, form so-called cysts as permanent forms of survival that are excreted with the stool and can also contain Legionella. The legionella find the best conditions for survival in the infectious amoebic cysts, as they are relatively well protected from dehydration and pollutants. Survival in the cysts offers a good guarantee for the permanent existence of the bacteria, because the bacteria do not form spores or other persistent forms.
If the cysts are ingested by humans or animals, the bacteria in the digestive tract are released again and can cause new legionellosis. The disease is more or less independent of the amoebic dysentery caused by the amoebic cysts. It is a kind of double infection with two different pathogens.
Analogous to survival in the amoeba, the pathogen also knows how to avoid dissolution in the phagocytes after their ingestion by producing certain enzymes and exotoxins and instead to benefit from the protection of the phagocytes and their further transport.
Illnesses & ailments
Legionella are almost ubiquitous, but the dangers they pose are mainly limited to a few species such as Legionella pneumophila. They run the risk of developing Legionnaires' disease or the less dangerous Pontiac fever.
The risk of infection depends very much on the bacterial density and the status of your own immune system. People with a weakened immune system or an artificially suppressed immune system are particularly at risk, which can be necessary after an organ transplant to avoid a rejection reaction.
Chemotherapy or radiation therapy to accompany cancer treatment also temporarily weakens the immune system, so that the risk of infection increases temporarily.
Experience has shown that infections with Legionnaires' disease are occasionally endemic in spatially limited areas. The endemic infections are mostly based on a high concentration of the pathogen at certain points. For example, if the hot water supply is improperly handled, containers and pipes are predestined for an accumulation of legionella, if the water is not heated to values above 60 degrees Celsius and the water reservoirs are also idle. This applies to schools, for example, whose hot water supply is not only not used on weekends, but the temperature is also lowered to values that offer optimal development opportunities for the pathogens to save costs.
In the past, there were also endemic infections from air conditioning systems in public buildings and hotels when the water separators in the system turned out to be a breeding ground for infectious Legionella. The germs were then evenly distributed throughout the buildings by the air conditioning system. A precautionary use of technical systems, which do not give legionella any opportunity to multiply exceptionally, therefore provides effective protection against infection.


.jpg)









.jpg)



.jpg)

.jpg)