Despite all the information, many women still shy away from going to the gynecologist, which is necessary in their own interest. Even many mothers unfortunately fail to see the necessary controls after giving birth and, out of carelessness or false shame, miss the mandatory follow-up examination. If, however, the daughter complains of abdominal complaints or has vaginal discharge at a young age, then, unfortunately, the fear of a doctor's visit usually wins out because the mothers believe, based on outdated ideas, that they should be ashamed of their child.
No shame at the gynecologist

Perhaps some of them are just forcing themselves to make a shameful question in the medical consultation about what "that" means, or whether something should be done "about it". But we can't help that way. As before any treatment, the doctor must make the diagnosis himself and the causes of the disease must be researched. This is especially true for the discharge from the vagina (fluorine), which is not a self-contained clinical picture, although we gynecologists have been dealing with it for a long time and occurs in more than 50 percent of our patients. There are numerous causes for the occurrence of fluorine, and it is imperative to find out the specific one from the numerous possible origins.
This already shows that no universal remedy can and should not be prescribed against the discharge, that every treatment must be adapted to the individual circumstances of the individual patient. This applies not only to the adult, but also to the child. That is why the attitude that you cannot take a child to the gynecologist is completely untenable. Even if a child's discharge is in many cases an everyday matter that should not be assessed as particularly tragic, it must be medically investigated and treated early, seriously and consistently.
Vaginal diseases in children and adolescents
Even in the newborn girl, we can often observe a white-slimy secretion on the outer genital area in the first few days, similar to a jelly-like mass that resembles the vaginal discharge in later years.
This is a slight, natural inflammation with the rejection of the finest surface cells at the end of the maternal hormone effect, which can also cause sparse bleeding from the child's vagina or uterine lining towards the end of the first week of life. The actual fluorine that occurs in infants and later is an increased fluid secretion from the area in front of the vaginal entrance (vulva), from the vaginal mucosa or from parts of the uterus.
It must be taken into account that the vaginal mucosa is normally never dry and contains germs from the hymen (hymen) to the outer cervix and the vaginal vaults even in a healthy state. An actually germ-free zone only begins from the cervix upwards, as long as no diseases or pregnancies have changed the balance of the vaginal secretions.
The presence of vaginal bacteria is by no means pathological. These germs, also called "Döderlein bacteria" after their discoverer and their shape, belong to the lactic acid bacteria that produce fermentation lactic acid from the starch components of decaying cells. However, starch, vaginal bacteria and lactic acid, together with fluid secretion, form the normal vaginal secretion, in which most foreign bacteria perish. Therefore, one rightly speaks of an anatomical and functional protective mechanism of the vagina as a result of constant self-cleaning. Every shift within this bacterial flora leads to pathological symptoms and thus to discharge.
Up until the first few years after the Second World War, before the widespread use of antibiotics, vaginal inflammation caused by gonorrhea (gonorrhea) was in the foreground of childhood diseases of fluorine in infants and toddlers. Like gonorrheic eye inflammation in infants, it can develop during childbirth when a woman suffers from an unnoticed, untreated gonorrhea.
This inflammation is seldom immediately noticeable in newborns and usually only appears after about two to three weeks, often not until they are two years old. Sometimes a direct transmission of the infection is possible by using the same bath sponges, the same bath water or shared hand towels, although this route is less common. In a fresh state, the diagnosis of this disease can often be made by the doctor with the naked eye, even before the typical pathogens, the gonococci, can be detected in the laboratory.
The great labia are reddened and covered with creamy, yellow-green pus; then in the little girl's laundry one finds yellow fleece. If this inflammation goes unnoticed and untreated, it becomes chronic; the discharge subsides and is finally barely noticeable. It is also typical that, before puberty, the child's vaginal mucous membrane reacts particularly frequently in an inflammatory manner, while in adult women it is primarily the urethral, uterine and rectal mucous membrane that is affected and the vagina itself remains insensitive.
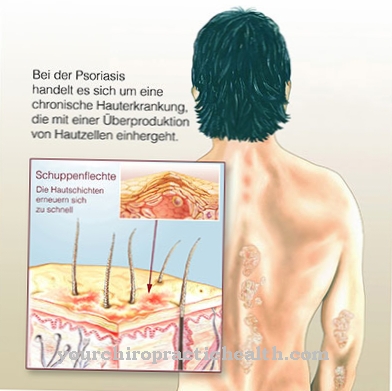
Another common, pathological disorder is the so-called vulvitis simplex, a "simple" vaginal inflammation in which only a small amount of watery-slimy discharge is observed. Even the inflammation is hardly apparent, and in particular the urethral opening and mucous membrane are not involved in the reddening. This is often an accompanying symptom of an innate, increased irritability of the skin and mucous membranes, so that eczema or itchy lichen on the rest of the body, mainly in the folds of the groin, occur at the same time. In this case, a predominantly plant-based diet prescribed by the doctor will reduce the disturbances.
Purulent fluorine can also occur in the wake of acute infectious diseases such as diphtheria, measles, smallpox, typhoid, chickenpox or rose. However, once the disease heals, it subsides again. Where there are also locally irritating causes, for example worms, poor hygiene, scratching or masturbation with unclean hands, vaginal discharge is more common and more noticeable.
Foreign bodies in the vagina also promote phenomena of this kind. We even find this in two- to three-year-old girls whose curiosity about their bodies is very great and who not only make small objects disappear in the nose and ears while playing. Almost two thirds of the cases of fluorine in children are infections of the vaginal secretions caused by "everyday" germs, which are mostly harmless and can be combated in a short time.
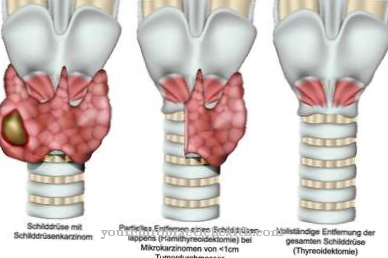
Finally, mild puberty fluorine can occur in older girls, which is usually also harmless. Since other diseases can hide behind the discharge, for example urogenital tuberculosis, if there are any signs of fluorine, you should consult a specialist immediately.
No danger for girls at the gynecologist
We can dispel the fears that the gynecological examination is not yet reasonable for a child because it cannot be carried out gently enough and would result in an injury to the hymen. For toddlers and toddlers, an ear speculum is sufficient to carry out a certain assessment of the vaginal mucosa including the removal of secretions.
The examination from the anus is also gently possible in children, which makes it possible to determine whether the organs in the small pelvis are in order. In addition, the gynecologist has very small special mirrors available for examining children, which are harmless and leave the hymen intact when the girl is relaxed and calm.
In passing, however, the question may also be asked what may harm the child more: a disease that has been delayed with the risk of inflammation that rises up into the fallopian tubes and thus later childlessness or a possibly no longer preserved hymen, which today is probably no longer a prerequisite for one Marriage can do.
In most cases, a very simple treatment relieves the girl from her unpleasant ailments, for which the gynecologist can also call on maternal help. Whether it is, for example, the application of external ointments, medicinal baths, taking certain medications or instilling certain solutions into the vagina, must be prescribed by a specialist according to the respective illness.
In general, the same principles apply to infantile fluids as to adult women: early treatment, exact compliance with medical advice and punctual re-presentation during the consultation hour. In this way the girls can be freed from the by no means embarrassing suffering.











.jpg)

.jpg)